Ch 6: States of Consciousness

States of Consciousness
Our lives involve regular, dramatic changes in the degree to which we are aware of our surroundings and our internal states. While awake, we feel alert and aware of the many important things going on around us. Our experiences change dramatically while we are in deep sleep and once again when we are dreaming. Sometimes, we seek to alter our awareness and experience by using psychoactive drugs; that is, drugs that alter the central nervous system and produce a change of consciousness or a deep meditative state. Consciousness is an awareness of external and internal stimuli. As discussed in the module on the biology of psychology, the brain activity during different phases of consciousness produces characteristic brain waves, which can be observed by electroencephalography (EEG) and other types of analysis.
This chapter will discuss states of consciousness with a particular emphasis on sleep. You’ll learn about the different stages of sleep, sleep disorders as well as the altered states of consciousness produced by psychoactive drugs, hypnosis, and meditation.
Consciousness and Rhythms
 Are you tired? Have you ever pulled an all-nighter? How did you feel the next day? Do you think your lack of sleep impacted your behavior? Chances are, you could answer that question with a resounding, “yes!”. Because psychologists are interested in mental processes and behavior, it’s essential to study consciousness, or our awareness, as humans. States of consciousness vary over the course of the day and throughout our lives, and sleep plays a major role in alertness levels. Important factors in daily changes in consciousness are biological rhythms, and, more specifically, the circadian rhythms generated by the suprachiasmatic nucleus. Typically, our biological clocks are aligned with our external environment, and light tends to be an important cue in setting this clock. When people travel across multiple time zones or work rotating shifts, they can experience disruptions of their circadian cycles that can lead to insomnia, sleepiness, and decreased alertness. If people go extended periods of time without sleep, they will accrue a sleep debt and potentially experience a number of adverse psychological and physiological consequences.
Are you tired? Have you ever pulled an all-nighter? How did you feel the next day? Do you think your lack of sleep impacted your behavior? Chances are, you could answer that question with a resounding, “yes!”. Because psychologists are interested in mental processes and behavior, it’s essential to study consciousness, or our awareness, as humans. States of consciousness vary over the course of the day and throughout our lives, and sleep plays a major role in alertness levels. Important factors in daily changes in consciousness are biological rhythms, and, more specifically, the circadian rhythms generated by the suprachiasmatic nucleus. Typically, our biological clocks are aligned with our external environment, and light tends to be an important cue in setting this clock. When people travel across multiple time zones or work rotating shifts, they can experience disruptions of their circadian cycles that can lead to insomnia, sleepiness, and decreased alertness. If people go extended periods of time without sleep, they will accrue a sleep debt and potentially experience a number of adverse psychological and physiological consequences.
Consciousness and Rhythms
Learning Objectives
- Describe consciousness and circadian rhythms
- Explain disruptions in biological rhythms, including sleep debt
Consciousness and Biological Rhythms
Consciousness describes our awareness of internal and external stimuli. Awareness of internal stimuli includes feeling pain, hunger, thirst, sleepiness, and being aware of our thoughts and emotions. Awareness of external stimuli includes seeing the light from the sun, feeling the warmth of a room, and hearing the voice of a friend.
We experience different states of consciousness and different levels of awareness on a regular basis. We might even describe consciousness as a continuum that ranges from full awareness to a deep sleep. Sleep is a state marked by relatively low levels of physical activity and reduced sensory awareness that is distinct from periods of rest that occur during wakefulness. Wakefulness is characterized by high levels of sensory awareness, thought, and behavior. In between these extremes are states of consciousness related to daydreaming, intoxication as a result of alcohol or other drug use, meditative states, hypnotic states, and altered states of consciousness following sleep deprivation. We might also experience unconscious states of being via drug-induced anesthesia for medical purposes. Often, we are not completely aware of our surroundings, even when we are fully awake. For instance, have you ever daydreamed while driving home from work or school without really thinking about the drive itself? You were capable of engaging in the all of the complex tasks involved with operating a motor vehicle even though you were not aware of doing so. Many of these processes, like much of psychological behavior, are rooted in our biology.
Biological Rhythms
Biological rhythms are internal rhythms of biological activity. A woman’s menstrual cycle is an example of a biological rhythm—a recurring, cyclical pattern of bodily changes. One complete menstrual cycle takes about 28 days—a lunar month—but many biological cycles are much shorter. Biological rhythms such as the menstrual cycle are called infradian rhythms because they last longer than 24 hours, and others that last less than 24 hours are called ultradian rhythms. Changes in body temperature and alertness that fluctuate cyclically over a 24-hour period (Figure 2) are examples of a circadian rhythm. A circadian rhythm is a biological rhythm that takes place over a period of about 24 hours. Alertness is associated with higher body temperatures, and sleepiness with lower body temperatures.

Our sleep-wake cycle, which is linked to our environment’s natural light-dark cycle, is perhaps the most obvious example of a circadian rhythm, but we also have daily fluctuations in heart rate, blood pressure, blood sugar, and body temperature. Some circadian rhythms play a role in changes in our state of consciousness.
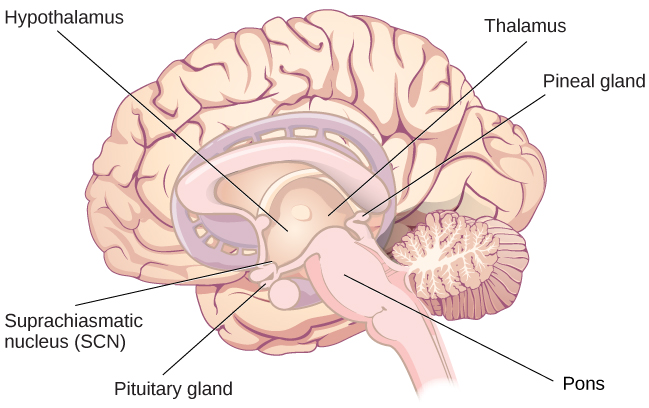
Research indicates that humans (as well as other animals and plants) have a biological clock, or an innate timing device, comprised of specific molecules (proteins) that interact in cells throughout the body. Biological clocks are found in nearly every tissue and organ. Researchers have identified similar genes in people, fruit flies, mice, fungi, and several other organisms that are responsible for making the clock’s components. In the brain, the hypothalamus, which lies above the pituitary gland, is a main center of homeostasis. Homeostasis is the tendency to maintain a balance, or optimal level, within a biological system.

Figure 3. The suprachiasmatic nucleus (SCN) serves as the brain’s clock mechanism. The clock sets itself with light information received through projections from the retina.
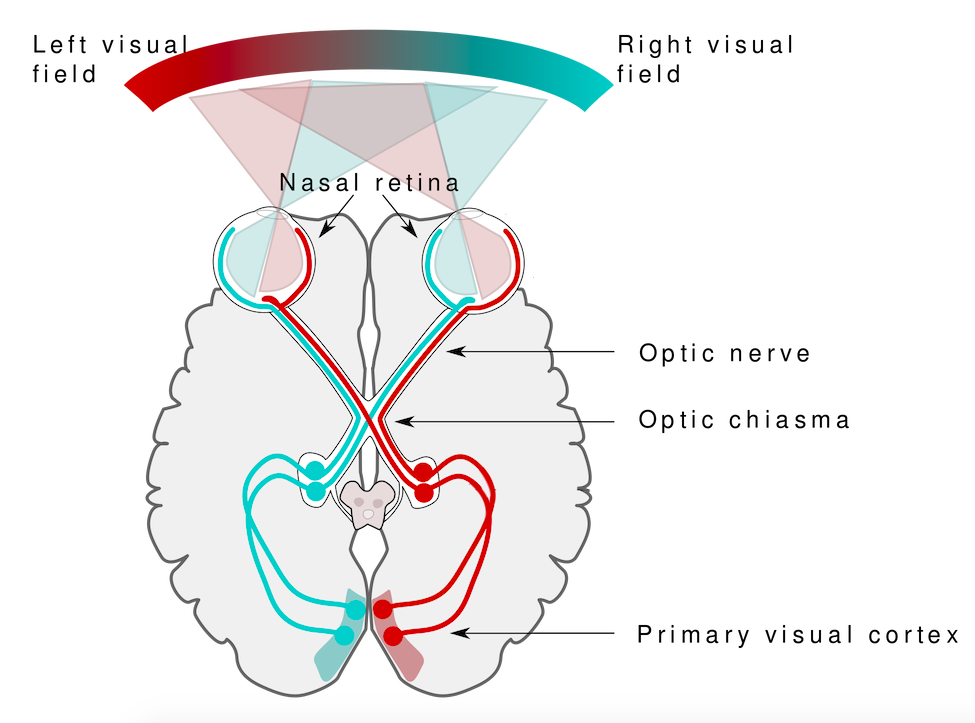
In people, the brain’s clock mechanism is located in an area of the hypothalamus known as the suprachiasmatic nucleus (SCN). The SCN is comprised of about 20,000 nerve cells. The axons of light-sensitive neurons in the retina provide information to the SCN based on the amount of light present, allowing this internal clock to be synchronized with the outside world (Klein, Moore, & Reppert, 1991; Welsh, Takahashi, & Kay, 2010) (Figure 3).
Watch It: Circadian Rhythms
Watch this brief video describing circadian rhythms and how they affect sleep.
Try It
Think It Over
Try It
Psychology in Real Life: Consciousness and Blindsight
Blindsight
What do you think would happen if your occipital lobes were damaged? Back in the 1970s, most scientists and physicians would have said, “you would become blind.” It turns out that the answer is more complicated than that.
When he was 8-years old, Graham Young from Oxford, England, was injured in a bicycle accident. Afterwards, he reported that parts of his vision were gone. He told his doctors that he could no longer see anything to the right of his center of vision with either his left or right eye. The left side of his visual world in both eyes was normal. Although he says that he would sometimes walk into objects to his right because he couldn’t see them, when tested fifteen years later, an optician discovered that Mr. Young seemed to respond to visual movements in his “blind” area.
Graham Young was put into contact with Psychologists Larry Weiskrantz and Elizabeth Warrington, who had worked previously with a person (known as DB) who seemed to have a similar ability to see despite blindness. DB could report shapes and colors, movement and the orientation of objects despite claiming that he could see nothing. He said that he was guessing, but he was usually right about colors and shapes and other characteristics of the objects.
Before we go on, please take a moment to theorize about what might be going on with Graham Young and DB.
Try It
People with blindsight have been tested for their ability to detect color differences, brightness changes, the ability to discriminate between various shapes, as well as tracking movement. Critically, people with blindsight have the conscious experience of blindness, often feeling like they are guessing despite their high level of accuracy.
Watch It: Blindsight In Action
Here is a brief video of the man who experiences complete blindness because his visual cortex in both hemispheres has been damaged. The researchers (including Dr. Weiskrantz, mentioned above) set up an obstacle course for the man (whose face is blurred to protect his privacy). Watch how well he moves through the objects without help. The man behind him is just there as a safety precaution.
How can blindsight happen?
Your conscious experience of the world around you, of the choices and decisions you make, and of the emotions and attitudes that motivate you are not the totality of your mental activity or of your brain’s processing of information. Many, perhaps most, psychologists believe that consciousness is only a small part of your total cognitive activity.[1]
A person is considered to be blind if he or she has no conscious experience of the visual world. This conscious experience is based on the flow of information from the eyes through the thalamus in the middle of the brain to the primary visual cortex in the occipital lobe at the back of the brain. If the primary visual cortex is damaged or fails to receive input due to disruption of visual pathway, then the person will not “see” the objects and events that we normally associate with vision.

Blindsight occurs because the visual system has a primary pathway (retina to thalamus to primary visual cortex), but it also has secondary pathways (retina to thalamus to other brain areas). These “other brain areas” include parts of the frontal lobe that guide eye movements, parts of the midbrain that help guide visual attention, and parts of the occipital lobe that process features of the visual perception, including shape, movement, and color.[2]
The existence of visual processing areas for isolated features of vision and the fact that these areas get some direct visual information (i.e, input that does not first go to the primary visual cortex) means that it is possible for a person to respond accurately to questions about color or motion or shape without consciously “seeing” the objects that have color or shape or are moving.
Try It
Watch It: Examining Blindsight
You can see Graham Young as he is tested in the lab in this video that shows him along with psychologist Larry Weizkrantz. The video clip (watch just the first 5.5 minutes), from a program hosted by neurologist V. S. Ramachandran, goes on to explain a theory as to why blindsight occurs.
You can view the transcript for “Part 3 – Phantoms In The Brain (Episode 1)” here (opens in new window).
It is important to remember that YOU have these same “unconscious” pathways in your visual system. That means your conscious experience of the visual world may not include all of the visual information you are processing. In other words, you may “know” more than you “see”.
Blindsight is not the only condition that involves unconscious or low-consciousness processing. Other neurological syndromes that have an unconscious element include amnesia, hemispatial neglect, dyslexia, aphasia, and various agnosias.[3]
Creating Blindsight in the Laboratory
Wouldn’t it be great if we could produce blindsight in the laboratory, in order to better understand visual processing and conscious experience? Maybe with college student volunteers as our subjects? Crazy idea?

It turns out, researchers have already done it. Using precisely aimed magnetic pulses, researchers can temporarily disrupt specific areas of the primary visual cortex—the area responsible for conscious vision—without injury. This “blindness” lasts only a fraction of a second, after which vision returns to normal. Would you volunteer to be a participant?
Let’s look at how this works.
TMS: Transcranial Magnetic Stimulation
Transcranial magnetic stimulation (TMS) is a procedure used to stimulate neurons in the brain. A device referred to as a “wand” contains an electric coil that generates a magnetic field that in turn creates a small electric current in the brain.[4] The electric current induces neurons (brain cells) to produce neural signals called action potentials. When action potentials are produced in normal brain processes, they allow neurons to communicate with one another. However, when action potentials are induced by an outside force—here by the TMS wand—they are meaningless and temporarily interfere with communication between neurons. If only a single pulse of electromagnetic energy is produced, then the disruption of the neurons in the targeted region lasts only a fraction of a second. Multiple pulses, called repetitive TMS (rTMS), can produce longer lasting effects. In fact, rTMS is now used by therapists as a treatment for depression and neuropathic pain.
The TMS pulse can be aimed very precisely at a small area of the brain. When the target is the primary visual cortex in the occipital lobe, the TMS pulse can be focused to interfere with neural communication in a tiny region of the of the visual field—so small and occurring for such a short time that you would not even notice. However brief the duration or tiny the affected area, the person receiving the TMS pulse is temporary blind in a small part of the visual field.
This section has been about consciousness awareness. It is common to assume that everything we know about the world around us and about our own thoughts and internal experiences must go through the doorway of our conscious mind. Evidence from blindsight is just one of several lines of research that shows that we process more information than we are aware of. Learning just how much this unconscious information can influence our thoughts and actions, our preferences and beliefs, is an important challenge for the rising generation of scientists.
When Biological Clocks Get Disrupted
Disruptions of Normal Sleep
Whether lark, owl, or somewhere in between, there are situations in which a person’s circadian clock gets out of synchrony with the external environment. One way that this happens involves traveling across multiple time zones. When we do this, we often experience jet lag. Jet lag is a collection of symptoms that results from the mismatch between our internal circadian cycles and our environment. These symptoms include fatigue, sluggishness, irritability, and insomnia (i.e., a consistent difficulty in falling or staying asleep for at least three nights a week over a month’s time) (Roth, 2007).
Individuals who do rotating shift work are also likely to experience disruptions in circadian cycles. Rotating shift work refers to a work schedule that changes from early to late on a daily or weekly basis. For example, a person may work from 7:00 a.m. to 3:00 p.m. on Monday, 3:00 a.m. to 11:00 a.m. on Tuesday, and 11:00 a.m. to 7:00 p.m. on Wednesday. In such instances, the individual’s schedule changes so frequently that it becomes difficult for a normal circadian rhythm to be maintained. This often results in sleeping problems, and it can lead to signs of depression and anxiety. These kinds of schedules are common for individuals working in health care professions and service industries, and they are associated with persistent feelings of exhaustion and agitation that can make someone more prone to making mistakes on the job (Gold et al., 1992; Presser, 1995).
Rotating shift work has pervasive effects on the lives and experiences of individuals engaged in that kind of work, which is clearly illustrated in stories reported in a qualitative study that researched the experiences of middle-aged nurses who worked rotating shifts (West, Boughton & Byrnes, 2009). Several of the nurses interviewed commented that their work schedules affected their relationships with their family. One of the nurses said,
If you’ve had a partner who does work regular job 9 to 5 office hours . . . the ability to spend time, good time with them when you’re not feeling absolutely exhausted . . . that would be one of the problems that I’ve encountered. (West et al., 2009, p. 114)
While disruptions in circadian rhythms can have negative consequences, there are things we can do to help us realign our biological clocks with the external environment. Some of these approaches, such as using a bright light as shown in Figure 7, have been shown to alleviate some of the problems experienced by individuals suffering from jet lag or from the consequences of rotating shift work. Because the biological clock is driven by light, exposure to bright light during working shifts and dark exposure when not working can help combat insomnia and symptoms of anxiety and depression (Huang, Tsai, Chen, & Hsu, 2013).

Insufficient Sleep
When people have difficulty getting sleep due to their work or the demands of day-to-day life, they accumulate a sleep debt. A person with a sleep debt does not get sufficient sleep on a chronic basis. The consequences of sleep debt include decreased levels of alertness and mental efficiency. Interestingly, since the advent of electric light, the amount of sleep that people get has declined. While we certainly welcome the convenience of having the darkness lit up, we also suffer the consequences of reduced amounts of sleep because we are more active during the nighttime hours than our ancestors were. As a result, many of us sleep less than 7–8 hours a night and accrue a sleep debt. While there is tremendous variation in any given individual’s sleep needs, the National Sleep Foundation (n.d.) cites research to estimate that newborns require the most sleep (between 12 and 18 hours a night) and that this amount declines to just 7–9 hours by the time we are adults.
If you lie down to take a nap and fall asleep very easily, chances are you may have sleep debt. Given that college students are notorious for suffering from significant sleep debt (Hicks, Fernandez, & Pelligrini, 2001; Hicks, Johnson, & Pelligrini, 1992; Miller, Shattuck, & Matsangas, 2010), chances are you and your classmates deal with sleep debt-related issues on a regular basis. The table below shows recommended amounts of sleep at different ages.
| Age | Nightly Sleep Needs |
|---|---|
| 0–3 months | 12–18 hours |
| 3 months–1 year | 14–15 hours |
| 1–3 years | 12–14 hours |
| 3–5 years | 11–13 hours |
| 5–10 years | 10–11 hours |
| 10–18 years | 8–10 hours |
| 18 and older | 7–9 hours |
Sleep debt and sleep deprivation have significant negative psychological and physiological consequences. As mentioned earlier, lack of sleep can result in decreased mental alertness and cognitive function. In addition, sleep deprivation often results in depression-like symptoms. These effects can occur as a function of accumulated sleep debt or in response to more acute periods of sleep deprivation. It may surprise you to know that sleep deprivation is associated with obesity, increased blood pressure, increased levels of stress hormones, and reduced immune functioning (Banks & Dinges, 2007). Furthermore, individuals suffering from sleep deprivation can also put themselves and others at risk when they put themselves behind the wheel of a car or work with dangerous machinery. Some research suggests that sleep deprivation affects cognitive and motor function as much as, if not more than, alcohol intoxication (Williamson & Feyer, 2000).

The amount of sleep we get varies across the lifespan. When we are very young, we spend up to 16 hours a day sleeping. As we grow older, we sleep less. In fact, a meta-analysis, which is a study that combines the results of many related studies, conducted within the last decade indicates that by the time we are 65 years old, we average fewer than 7 hours of sleep per day (Ohayon, Carskadon, Guilleminault, & Vitiello, 2004). As the amount of time we sleep varies over our lifespan, presumably the sleep debt would adjust accordingly.
Try It
Think It Over
Try It
Sleep and Dreams
 We devote a very large portion of time to sleep, and our brains have complex systems that control various aspects of sleep. Several hormones important for physical growth and maturation are secreted during sleep. While the reason we sleep remains something of a mystery, there is some evidence to suggest that sleep is very important to learning and memory.
We devote a very large portion of time to sleep, and our brains have complex systems that control various aspects of sleep. Several hormones important for physical growth and maturation are secreted during sleep. While the reason we sleep remains something of a mystery, there is some evidence to suggest that sleep is very important to learning and memory.
You may not feel particularly busy while you sleep, but you’ll learn in this section that your brain and body are quite active. You pass through four different stages of sleep. In this section, you’ll learn more about these sleep stages, dreaming, and sleep disorders.
Sleep and Dreams
Learning Objectives
- Describe areas of the brain and hormone secretions involved in sleep
- Describe several theories (adaptive and cognitive) aimed at explaining the function of sleep
- Differentiate between REM and non-REM sleep
- Describe the stages of sleep
- Describe and differentiate between theories on why we dream
- Describe the symptoms and treatments for insomnia, sleep apnea, and narcolepsy
Sleep and Why We Sleep
We spend approximately one-third of our lives sleeping. Given the average life expectancy for U.S. citizens falls between 73 and 79 years old (Singh & Siahpush, 2006), we can expect to spend approximately 25 years of our lives sleeping. Some animals never sleep (e.g., several fish and amphibian species); other animals can go extended periods of time without sleep and without apparent negative consequences (e.g., dolphins); yet some animals (e.g., rats) die after two weeks of sleep deprivation (Siegel, 2008). Why do we devote so much time to sleeping? Is it absolutely essential that we sleep? This section will consider these questions and explore various explanations for why we sleep.
What is Sleep?
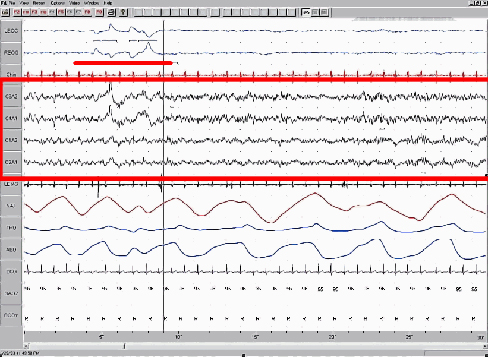
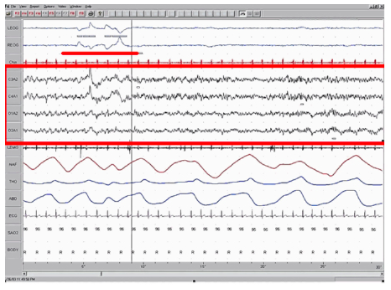
You have read that sleep is distinguished by low levels of physical activity and reduced sensory awareness. As discussed by Siegel (2008), a definition of sleep must also include mention of the interplay of the circadian and homeostatic mechanisms that regulate sleep. Homeostatic regulation of sleep is evidenced by sleep rebound following sleep deprivation. Sleep rebound refers to the fact that a sleep-deprived individual will tend to fall asleep faster during subsequent opportunities for sleep. Sleep is characterized by certain patterns of activity of the brain that can be visualized using electroencephalography (EEG), and different phases of sleep can be differentiated using EEG as well (Figure 9).
Sleep-wake cycles seem to be controlled by multiple brain areas acting in conjunction with one another. Some of these areas include the thalamus, the hypothalamus, and the pons. As already mentioned, the hypothalamus contains the SCN—the biological clock of the body—in addition to other nuclei that, in conjunction with the thalamus, regulate slow-wave sleep. The pons is important for regulating rapid eye movement (REM) sleep (National Institutes of Health, n.d.).
Sleep is also associated with the secretion and regulation of a number of hormones from several endocrine glands including: melatonin, follicle stimulating hormone (FSH), luteinizing hormone (LH), and growth hormone (National Institutes of Health, n.d.). You have read that the pineal gland releases melatonin during sleep (Figure 10). Melatonin is thought to be involved in the regulation of various biological rhythms and the immune system (Hardeland et al., 2006). During sleep, the pituitary gland secretes both FSH and LH which are important in regulating the reproductive system (Christensen et al., 2012; Sofikitis et al., 2008). The pituitary gland also secretes growth hormone, during sleep, which plays a role in physical growth and maturation as well as other metabolic processes (Bartke, Sun, & Longo, 2013).
Why Do We Sleep?
Given the central role that sleep plays in our lives and the number of adverse consequences that have been associated with sleep deprivation, one would think that we would have a clear understanding of why it is that we sleep. Unfortunately, this is not the case; however, several hypotheses have been proposed to explain the function of sleep.
Adaptive Function of Sleep
One popular hypothesis of sleep incorporates the perspective of evolutionary psychology. Evolutionary psychology is a discipline that studies how universal patterns of behavior and cognitive processes have evolved over time as a result of natural selection. Variations and adaptations in cognition and behavior make individuals more or less successful in reproducing and passing their genes to their offspring. One hypothesis from this perspective might argue that sleep is essential to restore resources that are expended during the day. Just as bears hibernate in the winter when resources are scarce, perhaps people sleep at night to reduce their energy expenditures. While this is an intuitive explanation of sleep, there is little research that supports this explanation. In fact, it has been suggested that there is no reason to think that energetic demands could not be addressed with periods of rest and inactivity (Frank, 2006; Rial et al., 2007), and some research has actually found a negative correlation between energetic demands and the amount of time spent sleeping (Capellini, Barton, McNamara, Preston, & Nunn, 2008).
Another evolutionary hypothesis of sleep holds that our sleep patterns evolved as an adaptive response to predatory risks, which increase in darkness. Thus we sleep in safe areas to reduce the chance of harm. Again, this is an intuitive and appealing explanation for why we sleep. Perhaps our ancestors spent extended periods of time asleep to reduce attention to themselves from potential predators. Comparative research indicates, however, that the relationship that exists between predatory risk and sleep is very complex and equivocal. Some research suggests that species that face higher predatory risks sleep fewer hours than other species (Capellini et al., 2008), while other researchers suggest there is no relationship between the amount of time a given species spends in deep sleep and its predation risk (Lesku, Roth, Amlaner, & Lima, 2006).
It is quite possible that sleep serves no single universally adaptive function, and different species have evolved different patterns of sleep in response to their unique evolutionary pressures. While we have discussed the negative outcomes associated with sleep deprivation, it should be pointed out that there are many benefits that are associated with adequate amounts of sleep. A few such benefits listed by the National Sleep Foundation (n.d.) include maintaining healthy weight, lowering stress levels, improving mood, and increasing motor coordination, as well as a number of benefits related to cognition and memory formation.
Cognitive Function of Sleep
Another theory regarding why we sleep involves sleep’s importance for cognitive function and memory formation (Rattenborg, Lesku, Martinez-Gonzalez, & Lima, 2007). Indeed, we know sleep deprivation results in disruptions in cognition and memory deficits (Brown, 2012), leading to impairments in our abilities to maintain attention, make decisions, and recall long-term memories. Moreover, these impairments become more severe as the amount of sleep deprivation increases (Alhola & Polo-Kantola, 2007). Furthermore, slow-wave sleep after learning a new task can improve resultant performance on that task (Huber, Ghilardi, Massimini, & Tononi, 2004) and seems essential for effective memory formation (Stickgold, 2005). Understanding the impact of sleep on cognitive function should help you understand that cramming all night for a test may be not effective and can even prove counterproductive.
Watch It
Watch this video to learn more about the function of sleep and the harmful effects of sleep deprivation.
Sleep has also been associated with other cognitive benefits. Research indicates that included among these possible benefits are increased capacities for creative thinking (Cai, Mednick, Harrison, Kanady, & Mednick, 2009; Wagner, Gais, Haider, Verleger, & Born, 2004), language learning (Fenn, Nusbaum, & Margoliash, 2003; Gómez, Bootzin, & Nadel, 2006), and inferential judgments (Ellenbogen, Hu, Payne, Titone, & Walker, 2007). It is possible that even the processing of emotional information is influenced by certain aspects of sleep (Walker, 2009).
Watch It
Learn about the connection between memory and sleep in the following clip:
Try It
Think It Over
Try It
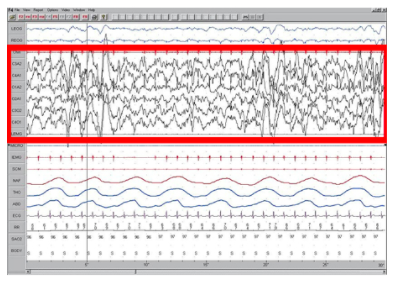
Stages of Sleep
Sleep is not a uniform state of being. Instead, sleep is composed of several different stages that can be differentiated from one another by the patterns of brain wave activity that occur during each stage. These changes in brain wave activity can be visualized using EEG and are distinguished from one another by both the frequency and amplitude of brain waves. Sleep can be divided into two different general phases: REM sleep and non-REM (NREM) sleep. Rapid eye movement (REM) sleep is characterized by darting movements of the eyes under closed eyelids. Brain waves during REM sleep appear very similar to brain waves during wakefulness, called beta waves. In contrast, non-REM (NREM) sleep[/pb_glossary] is subdivided into three stages distinguished from each other and from wakefulness by characteristic patterns of brain waves. The first three stages of sleep are NREM sleep, while the fourth and final stage of sleep is REM sleep. In this section, we will discuss each of these stages of sleep and their associated patterns of brain wave activity.
[Note that psychologists originally identified four stages of non-REM sleep, but these were revised in 2008, resulting in just three distinct phases of NREM sleep. You will see that stage 3 of NREM sleep is sometimes presented as both stage 3 and stage 4 in various texts.]
NREM Stages of Sleep
The first stage of NREM sleep is known as stage 1 sleep. [pb_glossary id="2553"]Stage 1 sleep is a transitional phase that occurs between wakefulness and sleep, the period during which we drift off to sleep. During this time, there is a slowdown in both the rates of respiration and heartbeat. In addition, stage 1 sleep involves a marked decrease in both overall muscle tension and core body temperature.
In terms of brain wave activity, stage 1 sleep is associated with both alpha and theta waves. The early portion of stage 1 sleep produces alpha waves, which are relatively low frequency (8–13Hz), high amplitude patterns of electrical activity (waves) that become synchronized. This pattern of brain wave activity resembles that of someone who is very relaxed, yet awake. As an individual continues through stage 1 sleep, there is an increase in theta wave activity. Theta waves are even lower frequency (4–7 Hz), higher amplitude brain waves than alpha waves. It is relatively easy to wake someone from stage 1 sleep; in fact, people often report that they have not been asleep if they are awoken during stage 1 sleep.

As we move into stage 2 sleep, the body goes into a state of deep relaxation. Theta waves still dominate the activity of the brain, but they are interrupted by brief bursts of activity known as sleep spindles (Figure 12). A sleep spindle is a rapid burst of higher frequency brain waves that may be important for learning and memory (Fogel & Smith, 2011; Poe, Walsh, & Bjorness, 2010). In addition, the appearance of K-complexes is often associated with stage 2 sleep. A K-complex is a very high amplitude pattern of brain activity that may in some cases occur in response to environmental stimuli. Thus, K-complexes might serve as a bridge to higher levels of arousal in response to what is going on in our environments (Halász, 1993; Steriade & Amzica, 1998).

Stage 3 of sleep is often referred to as deep sleep or slow-wave sleep because these stages are characterized by low frequency (up to 4 Hz), high amplitude delta waves (Figure 13). During this time, an individual’s heart rate and respiration slow dramatically. It is much more difficult to awaken someone from sleep during stage 3 than during earlier stages. Interestingly, individuals who have increased levels of alpha brain wave activity (more often associated with wakefulness and transition into stage 1 sleep) during stage 3 often report that they do not feel refreshed upon waking, regardless of how long they slept (Stone, Taylor, McCrae, Kalsekar, & Lichstein, 2008).
Try It
REM Sleep
As mentioned earlier, REM sleep is marked by rapid movements of the eyes. The brain waves associated with this stage of sleep are very similar to those observed when a person is awake, as shown in Figure 14, and this is the period of sleep in which dreaming occurs. It is also associated with paralysis of muscle systems in the body with the exception of those that make circulation and respiration possible. Therefore, no movement of voluntary muscles occurs during REM sleep in a normal individual; REM sleep is often referred to as paradoxical sleep because of this combination of high brain activity and lack of muscle tone. Like NREM sleep, REM has been implicated in various aspects of learning and memory (Wagner, Gais, & Born, 2001), although there is disagreement within the scientific community about how important both NREM and REM sleep are for normal learning and memory (Siegel, 2001).
If people are deprived of REM sleep and then allowed to sleep without disturbance, they will spend more time in REM sleep in what would appear to be an effort to recoup the lost time in REM. This is known as the REM rebound, and it suggests that REM sleep is also homeostatically regulated. Aside from the role that REM sleep may play in processes related to learning and memory, REM sleep may also be involved in emotional processing and regulation. In such instances, REM rebound may actually represent an adaptive response to stress in nondepressed individuals by suppressing the emotional salience of aversive events that occurred in wakefulness (Suchecki, Tiba, & Machado, 2012).
While sleep deprivation in general is associated with a number of negative consequences (Brown, 2012), the consequences of REM deprivation appear to be less profound (as discussed in Siegel, 2001). In fact, some have suggested that REM deprivation can actually be beneficial in some circumstances. For instance, REM sleep deprivation has been demonstrated to improve symptoms of people suffering from major depression, and many effective antidepressant medications suppress REM sleep (Riemann, Berger, & Volderholzer, 2001; Vogel, 1975).
It should be pointed out that some reviews of the literature challenge this finding, suggesting that sleep deprivation that is not limited to REM sleep is just as effective or more effective at alleviating depressive symptoms among some patients suffering from depression. In either case, why sleep deprivation improves the mood of some patients is not entirely understood (Giedke & Schwärzler, 2002). Recently, however, some have suggested that sleep deprivation might change emotional processing so that various stimuli are more likely to be perceived as positive in nature (Gujar, Yoo, Hu, & Walker, 2011). The hypnogram below (Figure 15) shows a person’s passage through the stages of sleep.

Try It
Think It Over
Try It
Dreams and Dreaming
Dreams
The meaning of dreams varies across different cultures and periods of time. By the late 19th century, German psychiatrist Sigmund Freud had become convinced that dreams represented an opportunity to gain access to the unconscious. By analyzing dreams, Freud thought people could increase self-awareness and gain valuable insight to help them deal with the problems they faced in their lives. Freud made distinctions between the manifest content and the latent content of dreams.
Manifest content is the actual content, or storyline, of a dream. Latent content, on the other hand, refers to the hidden meaning of a dream. For instance, if a woman dreams about being chased by a snake, Freud might have argued that this represents the woman’s fear of sexual intimacy, with the snake serving as a symbol of a man’s penis.
Freud was not the only theorist to focus on the content of dreams. The 20th century Swiss psychiatrist Carl Jung believed that dreams allowed us to tap into the collective unconscious. The collective unconscious, as described by Jung, is a theoretical repository of information he believed to be shared by everyone. According to Jung, certain symbols in dreams reflected universal archetypes with meanings that are similar for all people regardless of culture or location.
The sleep and dreaming researcher Rosalind Cartwright, however, believes that dreams simply reflect life events that are important to the dreamer. Unlike Freud and Jung, Cartwright’s ideas about dreaming have found empirical support. For example, she and her colleagues published a study in which women going through divorce were asked several times over a five month period to report the degree to which their former spouses were on their minds. These same women were awakened during REM sleep in order to provide a detailed account of their dream content. There was a significant positive correlation between the degree to which women thought about their former spouses during waking hours and the number of times their former spouses appeared as characters in their dreams (Cartwright, Agargun, Kirkby, & Friedman, 2006). Recent research (Horikawa, Tamaki, Miyawaki, & Kamitani, 2013) has uncovered new techniques by which researchers may effectively detect and classify the visual images that occur during dreaming by using fMRI for neural measurement of brain activity patterns, opening the way for additional research in this area.

Recently, neuroscientists have also become interested in understanding why we dream. For example, Hobson (2009) suggests that dreaming may represent a state of protoconsciousness. In other words, dreaming involves constructing a virtual reality in our heads that we might use to help us during wakefulness. Among a variety of neurobiological evidence, John Hobson cites research on lucid dreams as an opportunity to better understand dreaming in general. Lucid dreams are dreams in which certain aspects of wakefulness are maintained during a dream state. In a lucid dream, a person becomes aware of the fact that they are dreaming, and as such, they can control the dream’s content (LaBerge, 1990).
Theories on Dreaming
While the Freudian theory of dreaming may be the most well known, and Cartwright's suggestions on dreaming the most plausible, there are several other theories about the purpose of dreaming. The threat-simulation theory suggests that dreaming should be seen as an ancient biological defense mechanism. Dreams are thought to provide an evolutionary advantage because of their capacity to repeatedly simulate potential threatening events. This process enhances the neurocognitive mechanisms required for efficient threat perception and avoidance.
The expectation-fulfillment theory posits that dreaming serves to discharge emotional arousals (however minor) that haven't been expressed during the day. This practice frees up space in the brain to deal with the emotional arousals of the next day and allows instinctive urges to stay intact. In effect, the expectation is fulfilled (the action is "completed") in a metaphorical form so that a false memory is not created. This theory explains why dreams are usually forgotten immediately afterwards.
One prominent neurobiological theory of dreaming is the activation-synthesis theory, which states that dreams don't actually mean anything. They are merely electrical brain impulses that pull random thoughts and imagery from our memories. The theory posits that humans construct dream stories after they wake up, in a natural attempt to make sense of the nonsensical. However, given the vast documentation of the realistic aspects of human dreaming, as well as indirect experimental evidence that other mammals such as cats also dream, evolutionary psychologists have theorized that dreaming does indeed serve a purpose.
The continual-activation theory proposes that dreaming is a result of brain activation and synthesis. Dreaming and REM sleep are simultaneously controlled by different brain mechanisms. The hypothesis states that the function of sleep is to process, encode, and transfer data from short-term memory to long-term memory through a process called consolidation. However, there is not much evidence to back this up. NREM sleep processes the conscious-related memory (declarative memory), and REM sleep processes the unconscious related memory (procedural memory). The underlying assumption of continual-activation theory is that, during REM sleep, the unconscious part of the brain is busy processing procedural memory. Meanwhile, the level of activation in the conscious part of the brain descends to a very low level as the inputs from the senses are basically disconnected. This triggers the "continual-activation" mechanism to generate a data stream from the memory stores to flow through to the conscious part of the brain.
Watch It
Review the purpose and stages of sleep as well as the reasons why we dream in the following CrashCourse video:
Try It
Sleep Problems and Disorders
Many people experience disturbances in their sleep at some point in their lives. Depending on the population and sleep disorder being studied, between 30% and 50% of the population suffers from a sleep disorder at some point in their lives (Bixler, Kales, Soldatos, Kaels, & Healey, 1979; Hossain & Shapiro, 2002; Ohayon, 1997, 2002; Ohayon & Roth, 2002). This section will describe several sleep disorders as well as some of their treatment options.
Parasomnias
A parasomnia is one of a group of sleep disorders in which unwanted, disruptive motor activity and/or experiences during sleep play a role. Parasomnias can occur in either REM or NREM phases of sleep. Sleepwalking, restless leg syndrome, and night terrors are all examples of parasomnias (Mahowald & Schenck, 2000).
Sleepwalking
In sleepwalking, or somnambulism, the sleeper engages in relatively complex behaviors ranging from wandering about to driving an automobile. During periods of sleepwalking, sleepers often have their eyes open, but they are not responsive to attempts to communicate with them. Sleepwalking most often occurs during slow-wave sleep, but it can occur at any time during a sleep period in some affected individuals (Mahowald & Schenck, 2000).
Historically, somnambulism has been treated with a variety of pharmacotherapies ranging from benzodiazepines to antidepressants. However, the success rate of such treatments is questionable. Guilleminault et al. (2005) found that sleepwalking was not alleviated with the use of benzodiazepines. However, all of their somnambulistic patients who also suffered from sleep-related breathing problems showed a marked decrease in sleepwalking when their breathing problems were effectively treated.
Dig Deeper: A Sleepwalking Defense?
On January 16, 1997, Scott Falater sat down to dinner with his wife and children and told them about difficulties he was experiencing on a project at work. After dinner, he prepared some materials to use in leading a church youth group the following morning, and then he attempted repair the family’s swimming pool pump before retiring to bed. The following morning, he awoke to barking dogs and unfamiliar voices from downstairs. As he went to investigate what was going on, he was met by a group of police officers who arrested him for the murder of his wife (Cartwright, 2004; CNN, 1999).
Yarmila Falater’s body was found in the family’s pool with 44 stab wounds. A neighbor called the police after witnessing Falater standing over his wife’s body before dragging her into the pool. Upon a search of the premises, police found blood-stained clothes and a bloody knife in the trunk of Falater’s car, and he had blood stains on his neck.
Remarkably, Falater insisted that he had no recollection of hurting his wife in any way. His children and his wife’s parents all agreed that Falater had an excellent relationship with his wife and they couldn’t think of a reason that would provide any sort of motive to murder her (Cartwright, 2004).
Scott Falater had a history of regular episodes of sleepwalking as a child, and he had even behaved violently toward his sister once when she tried to prevent him from leaving their home in his pajamas during a sleepwalking episode. He suffered from no apparent anatomical brain anomalies or psychological disorders. It appeared that Scott Falater had killed his wife in his sleep, or at least, that is the defense he used when he was tried for his wife’s murder (Cartwright, 2004; CNN, 1999). In Falater’s case, a jury found him guilty of first degree murder in June of 1999 (CNN, 1999); however, there are other murder cases where the sleepwalking defense has been used successfully. As scary as it sounds, many sleep researchers believe that homicidal sleepwalking is possible in individuals suffering from the types of sleep disorders described below (Broughton et al., 1994; Cartwright, 2004; Mahowald, Schenck, & Cramer Bornemann, 2005; Pressman, 2007).
REM Sleep Behavior Disorder (RBD)
REM sleep behavior disorder (RBD) occurs when the muscle paralysis associated with the REM sleep phase does not occur. Individuals who suffer from RBD have high levels of physical activity during REM sleep, especially during disturbing dreams. These behaviors vary widely, but they can include kicking, punching, scratching, yelling, and behaving like an animal that has been frightened or attacked. People who suffer from this disorder can injure themselves or their sleeping partners when engaging in these behaviors. Furthermore, these types of behaviors ultimately disrupt sleep, although affected individuals have no memories that these behaviors have occurred (Arnulf, 2012).
This disorder is associated with a number of neurodegenerative diseases such as Parkinson’s disease. In fact, this relationship is so robust that some view the presence of RBD as a potential aid in the diagnosis and treatment of a number of neurodegenerative diseases (Ferini-Strambi, 2011). Clonazepam, an anti-anxiety medication with sedative properties, is most often used to treat RBD. It is administered alone or in conjunction with doses of melatonin (the hormone secreted by the pineal gland). As part of treatment, the sleeping environment is often modified to make it a safer place for those suffering from RBD (Zangini, Calandra-Buonaura, Grimaldi, & Cortelli, 2011).
Other Parasomnias
A person with restless leg syndrome has uncomfortable sensations in the legs during periods of inactivity or when trying to fall asleep. This discomfort is relieved by deliberately moving the legs, which, not surprisingly, contributes to difficulty in falling or staying asleep. Restless leg syndrome is quite common and has been associated with a number of other medical diagnoses, such as chronic kidney disease and diabetes (Mahowald & Schenck, 2000). There are a variety of drugs that treat restless leg syndrome: benzodiazepines, opiates, and anticonvulsants (Restless Legs Syndrome Foundation, n.d.).
Night terrors result in a sense of panic in the sufferer and are often accompanied by screams and attempts to escape from the immediate environment (Mahowald & Schenck, 2000). Although individuals suffering from night terrors appear to be awake, they generally have no memories of the events that occurred, and attempts to console them are ineffective. Typically, individuals suffering from night terrors will fall back asleep again within a short time. Night terrors apparently occur during the NREM phase of sleep (Provini, Tinuper, Bisulli, & Lagaresi, 2011). Generally, treatment for night terrors is unnecessary unless there is some underlying medical or psychological condition that is contributing to the night terrors (Mayo Clinic, n.d.).
Try It
Insomnia
While parasomnias are disorders related to the various stages of sleep, other sleep disorders, such as insomnia, are related to sleep in general. Insomnia is a consistent difficulty in falling or staying asleep, and is the most common of the sleep disorders. Individuals with insomnia often experience long delays between the times that they go to bed and actually fall asleep. In addition, these individuals may wake up several times during the night only to find that they have difficulty getting back to sleep. As mentioned earlier, one of the criteria for insomnia involves experiencing these symptoms for at least three nights a week for at least one month’s time (Roth, 2007).
It is not uncommon for people suffering from insomnia to experience increased levels of anxiety about their inability to fall asleep. This becomes a self-perpetuating cycle because increased anxiety leads to increased arousal, and higher levels of arousal make the prospect of falling asleep even more unlikely. Chronic insomnia is almost always associated with feeling overtired and may be associated with symptoms of depression.
There may be many factors that contribute to insomnia, including age, drug use, exercise, mental status, and bedtime routines. Not surprisingly, insomnia treatment may take one of several different approaches. People who suffer from insomnia might limit their use of stimulant drugs (such as caffeine) or increase their amount of physical exercise during the day. Some people might turn to over-the-counter (OTC) or prescribed sleep medications to help them sleep, but this should be done sparingly because many sleep medications result in dependence and alter the nature of the sleep cycle, and they can increase insomnia over time. Those who continue to have insomnia, particularly if it affects their quality of life, should seek professional treatment.
Some forms of psychotherapy, such as cognitive-behavioral therapy, can help sufferers of insomnia. Cognitive-behavioral therapy is a type of psychotherapy that focuses on cognitive processes and problem behaviors. The treatment of insomnia likely would include stress management techniques and changes in problematic behaviors that could contribute to insomnia (e.g., spending more waking time in bed). Cognitive-behavioral therapy has been demonstrated to be quite effective in treating insomnia (Savard, Simard, Ivers, & Morin, 2005; Williams, Roth, Vatthauer, & McCrae, 2013).
Sleep Apnea
Sleep apnea is defined by episodes during which a sleeper’s breathing stops. These episodes can last 10–20 seconds or longer and often are associated with brief periods of arousal. While individuals suffering from sleep apnea may not be aware of these repeated disruptions in sleep, they do experience increased levels of fatigue. Many individuals diagnosed with sleep apnea first seek treatment because their sleeping partners indicate that they snore loudly and/or stop breathing for extended periods of time while sleeping (Henry & Rosenthal, 2013). Sleep apnea is much more common in overweight people and is often associated with loud snoring. Surprisingly, sleep apnea may exacerbate cardiovascular disease (Sánchez-de-la-Torre, Campos-Rodriguez, & Barbé, 2012). While sleep apnea is less common in thin people, anyone, regardless of their weight, who snores loudly or gasps for air while sleeping, should be checked for sleep apnea.
While people are often unaware of their sleep apnea, they are keenly aware of some of the adverse consequences of insufficient sleep. Consider a patient who believed that as a result of his sleep apnea he “had three car accidents in six weeks. They were ALL my fault. Two of them I didn’t even know I was involved in until afterwards” (Henry & Rosenthal, 2013, p. 52). It is not uncommon for people suffering from undiagnosed or untreated sleep apnea to fear that their careers will be affected by the lack of sleep, illustrated by this statement from another patient, “I’m in a job where there’s a premium on being mentally alert. I was really sleepy… and having trouble concentrating…. It was getting to the point where it was kind of scary” (Henry & Rosenthal, 2013, p. 52).
There are two types of sleep apnea: obstructive sleep apnea and central sleep apnea. Obstructive sleep apnea occurs when an individual’s airway becomes blocked during sleep, and air is prevented from entering the lungs. In central sleep apnea, disruption in signals sent from the brain that regulate breathing cause periods of interrupted breathing (White, 2005).
One of the most common treatments for sleep apnea involves the use of a special device during sleep. A continuous positive airway pressure (CPAP) device includes a mask that fits over the sleeper’s nose and mouth, which is connected to a pump that pumps air into the person’s airways, forcing them to remain open, as shown in Figure 17. Some newer CPAP masks are smaller and cover only the nose. This treatment option has proven to be effective for people suffering from mild to severe cases of sleep apnea (McDaid et al., 2009). However, alternative treatment options are being explored because consistent compliance by users of CPAP devices is a problem. Recently, a new EPAP (excitatory positive air pressure) device has shown promise in double-blind trials as one such alternative (Berry, Kryger, & Massie, 2011).

Narcolepsy
Unlike the other sleep disorders described in this section, a person with narcolepsy cannot resist falling asleep at inopportune times. These sleep episodes are often associated with cataplexy, which is a lack of muscle tone or muscle weakness, and in some cases involves complete paralysis of the voluntary muscles. This is similar to the kind of paralysis experienced by healthy individuals during REM sleep (Burgess & Scammell, 2012; Hishikawa & Shimizu, 1995; Luppi et al., 2011). Narcoleptic episodes take on other features of REM sleep. For example, around one third of individuals diagnosed with narcolepsy experience vivid, dream-like hallucinations during narcoleptic attacks (Chokroverty, 2010).
Surprisingly, narcoleptic episodes are often triggered by states of heightened arousal or stress. The typical episode can last from a minute or two to half an hour. Once awakened from a narcoleptic attack, people report that they feel refreshed (Chokroverty, 2010). Obviously, regular narcoleptic episodes could interfere with the ability to perform one’s job or complete schoolwork, and in some situations, narcolepsy can result in significant harm and injury (e.g., driving a car or operating machinery or other potentially dangerous equipment).
Generally, narcolepsy is treated using psychomotor stimulant drugs, such as amphetamines (Mignot, 2012). These drugs promote increased levels of neural activity. Narcolepsy is associated with reduced levels of the signaling molecule hypocretin in some areas of the brain (De la Herrán-Arita & Drucker-Colín, 2012; Han, 2012), and the traditional stimulant drugs do not have direct effects on this system. Therefore, it is quite likely that new medications that are developed to treat narcolepsy will be designed to target the hypocretin system.
There is a tremendous amount of variability among sufferers, both in terms of how symptoms of narcolepsy manifest and the effectiveness of currently available treatment options. This is illustrated by McCarty’s (2010) case study of a 50-year-old woman who sought help for the excessive sleepiness during normal waking hours that she had experienced for several years. She indicated that she had fallen asleep at inappropriate or dangerous times, including while eating, while socializing with friends, and while driving her car. During periods of emotional arousal, the woman complained that she felt some weakness in the right side of her body. Although she did not experience any dream-like hallucinations, she was diagnosed with narcolepsy as a result of sleep testing. In her case, the fact that her cataplexy was confined to the right side of her body was quite unusual. Early attempts to treat her condition with a stimulant drug alone were unsuccessful. However, when a stimulant drug was used in conjunction with a popular antidepressant, her condition improved dramatically.
Try It
Think It Over
Try It
Drugs and Other States of Consciousness
 While we all experience altered states of consciousness in the form of sleep on a regular basis, some people use drugs and other substances that result in altered states of consciousness as well. This section will present information relating to the use of various psychoactive drugs and problems associated with such use. You'll also learned about other altered states of consciousness like hypnosis and meditation.
While we all experience altered states of consciousness in the form of sleep on a regular basis, some people use drugs and other substances that result in altered states of consciousness as well. This section will present information relating to the use of various psychoactive drugs and problems associated with such use. You'll also learned about other altered states of consciousness like hypnosis and meditation.
Watch It
This CrashCourse video gives an excellent overview of these altered states:
You can view the transcript "Altered States: Crash Course Psychology #10" here (opens in new window).
Drugs and Other States of Consciousness
Learning Objectives
- Describe how substance abuse disorders are diagnosed
- Explain how depressants impact nervous system activity
- Identify stimulants and describe how they affect the brain and body
- Identify opioids and describe how they impact the brain and behavior
- Describe hallucinogens and how they affect the brain and behavior
- Compare and contrast between depressants, stimulants, opioids, and hallucinogens
- Describe hypnosis and meditation
Psychoactive Drugs and Addiction
Substance Abuse Disorders
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) is used by clinicians to diagnose individuals suffering from various psychological disorders. Drug use disorders are addictive disorders, and the criteria for specific substance (drug) use disorders are described in DSM-5. A person who has a substance use disorder often uses more of the substance than they originally intended to and continues to use that substance despite experiencing significant adverse consequences. In individuals diagnosed with a substance use disorder, there is a compulsive pattern of drug use that is often associated with both physical and psychological dependence.
Physical dependence involves changes in normal bodily functions—the user will experience withdrawal from the drug upon cessation of use. In contrast, a person who has psychological dependence has an emotional, rather than physical, need for the drug and may use the drug to relieve psychological distress. Tolerance is linked to physiological dependence, and it occurs when a person requires more and more drug to achieve effects previously experienced at lower doses. Tolerance can cause the user to increase the amount of drug used to a dangerous level—even to the point of overdose and death.
Drug withdrawal includes a variety of negative symptoms experienced when drug use is discontinued. These symptoms usually are opposite of the effects of the drug. For example, withdrawal from sedative drugs often produces unpleasant arousal and agitation. In addition to withdrawal, many individuals who are diagnosed with substance use disorders will also develop tolerance to these substances. Psychological dependence, or drug craving, is a recent addition to the diagnostic criteria for substance use disorder in DSM-5. This is an important factor because we can develop tolerance and experience withdrawal from any number of drugs that we do not abuse. In other words, physical dependence in and of itself is of limited utility in determining whether or not someone has a substance use disorder.
Link to Learning
Read through this fascinating comic created by Stuart McMillen about psychologist's Bruce Alexander's Rat Park study on addiction.
For more information on Bruce Alexander's study and a better understanding of addiction, listen to Johann Hari's TED Talk, "Everything you think you know about addiction is wrong."
Drug Categories
The effects of all psychoactive drugs occur through their interactions with our endogenous neurotransmitter systems. Many of these drugs, and their relationships, are shown in Figure 19. As you have learned, drugs can act as agonists or antagonists of a given neurotransmitter system. An agonist facilitates the activity of a neurotransmitter system, and antagonists impede neurotransmitter activity.
The main categories of drugs are depressants, stimulants, and hallucinogens. You'll learn more about these types drugs next.

Try It
Alcohol and Other Depressants
Ethanol, which we commonly refer to as alcohol, is in a class of psychoactive drugs known as depressants (Figure 20). A depressant is a drug that tends to suppress central nervous system activity. Other depressants include barbiturates and benzodiazepines. These drugs share in common their ability to serve as agonists of the gamma-Aminobutyric acid (GABA) neurotransmitter system. Because GABA has a quieting effect on the brain, GABA agonists also have a quieting effect; these types of drugs are often prescribed to treat both anxiety and insomnia.

Acute alcohol administration results in a variety of changes to consciousness. Alcohol intoxication is measured for legal and medical uses in terms of Blood Alcohol Content (BAC). A BAC of 0.10 (0.10% or one-tenth of one percent) means that there are 0.10 g of alcohol for every 100 ml of blood. While a BAC of 0.0 is sober, in the United States a BAC of 0.08 is legally intoxicated, and above that is considered very impaired. BAC levels above 0.40 are potentially fatal. At rather low doses, alcohol use is associated with feelings of euphoria. As the dose increases, people report feeling sedated. Generally, alcohol is associated with decreases in reaction time and visual acuity, lowered levels of alertness, and reduction in behavioral control. With excessive alcohol use, a person might experience a complete loss of consciousness and/or difficulty remembering events that occurred during a period of intoxication (McKim & Hancock, 2013). In addition, if a pregnant woman consumes alcohol, her infant may be born with a cluster of birth defects and symptoms collectively called fetal alcohol spectrum disorder (FASD) or fetal alcohol syndrome (FAS).
With repeated use of many central nervous system depressants, such as alcohol, a person becomes physically dependent upon the substance and will exhibit signs of both tolerance and withdrawal. Psychological dependence on these drugs is also possible. Therefore, the abuse potential of central nervous system depressants is relatively high.
Drug withdrawal is usually an aversive experience, and it can be a life-threatening process in individuals who have a long history of very high doses of alcohol and/or barbiturates. This is of such concern that people who are trying to overcome addiction to these substances should only do so under medical supervision.
Try It
Stimulants
Stimulants are drugs that tend to increase overall levels of neural activity. Many of these drugs act as agonists of the dopamine neurotransmitter system. Dopamine activity is often associated with reward and craving; therefore, drugs that affect dopamine neurotransmission often have abuse liability. Drugs in this category include cocaine, amphetamines (including methamphetamine), cathinones (i.e., bath salts), MDMA (ecstasy), nicotine, and caffeine.
Dig Deeper: Crack Cocaine
Crack (Figure 21) is often considered to be more addictive than cocaine itself because it is smokable and reaches the brain very quickly. Crack is often less expensive than other forms of cocaine; therefore, it tends to be a more accessible drug for individuals from impoverished segments of society. During the 1980s, many drug laws were rewritten to punish crack users more severely than cocaine users. This led to discriminatory sentencing with low-income, inner-city minority populations receiving the harshest punishments. The wisdom of these laws has recently been called into question, especially given research that suggests crack may not be more addictive than other forms of cocaine, as previously thought (Haasen & Krausz, 2001; Reinerman, 2007).

Amphetamines have a mechanism of action quite similar to cocaine in that they block the reuptake of dopamine in addition to stimulating its release (Figure 22). While amphetamines are often abused, they are also commonly prescribed to children diagnosed with attention deficit hyperactivity disorder (ADHD). It may seem counterintuitive that stimulant medications are prescribed to treat a disorder that involves hyperactivity, but the therapeutic effect comes from increases in neurotransmitter activity within certain areas of the brain associated with impulse control.

In recent years, methamphetamine (meth) use has become increasingly widespread. Methamphetamine is a type of amphetamine that can be made from ingredients that are readily available (e.g., medications containing pseudoephedrine, a compound found in many over-the-counter cold and flu remedies). Despite recent changes in laws designed to make obtaining pseudoephedrine more difficult, methamphetamine continues to be an easily accessible and relatively inexpensive drug option (Shukla, Crump, & Chrisco, 2012).
The cocaine, amphetamine, cathinones, and MDMA users seek a euphoric high, feelings of intense elation and pleasure, especially in those users who take the drug via intravenous injection or smoking. Repeated use of these stimulants can have significant adverse consequences. Users can experience physical symptoms that include nausea, elevated blood pressure, and increased heart rate. In addition, these drugs can cause feelings of anxiety, hallucinations, and paranoia (Fiorentini et al., 2011). Normal brain functioning is altered after repeated use of these drugs. For example, repeated use can lead to overall depletion among the monoamine neurotransmitters (dopamine, norepinephrine, and serotonin). People may engage in compulsive use of these stimulant substances in part to try to reestablish normal levels of these neurotransmitters (Jayanthi & Ramamoorthy, 2005; Rothman, Blough, & Baumann, 2007).
Caffeine is another stimulant drug. While it is probably the most commonly used drug in the world, the potency of this particular drug pales in comparison to the other stimulant drugs described in this section. Generally, people use caffeine to maintain increased levels of alertness and arousal. Caffeine is found in many common medicines (such as weight loss drugs), beverages, foods, and even cosmetics (Herman & Herman, 2013). While caffeine may have some indirect effects on dopamine neurotransmission, its primary mechanism of action involves antagonizing adenosine activity (Porkka-Heiskanen, 2011).
While caffeine is generally considered a relatively safe drug, high blood levels of caffeine can result in insomnia, agitation, muscle twitching, nausea, irregular heartbeat, and even death (Reissig, Strain, & Griffiths, 2009; Wolt, Ganetsky, & Babu, 2012). In 2012, Kromann and Nielson reported on a case study of a 40-year-old woman who suffered significant ill effects from her use of caffeine. The woman used caffeine in the past to boost her mood and to provide energy, but over the course of several years, she increased her caffeine consumption to the point that she was consuming three liters of soda each day. Although she had been taking a prescription antidepressant, her symptoms of depression continued to worsen and she began to suffer physically, displaying significant warning signs of cardiovascular disease and diabetes. Upon admission to an outpatient clinic for treatment of mood disorders, she met all of the diagnostic criteria for substance dependence and was advised to dramatically limit her caffeine intake. Once she was able to limit her use to less than 12 ounces of soda a day, both her mental and physical health gradually improved. Despite the prevalence of caffeine use and the large number of people who confess to suffering from caffeine addiction, this was the first published description of soda dependence appearing in scientific literature.
Nicotine is highly addictive, and the use of tobacco products is associated with increased risks of heart disease, stroke, and a variety of cancers. Nicotine exerts its effects through its interaction with acetylcholine receptors. Acetylcholine functions as a neurotransmitter in motor neurons. In the central nervous system, it plays a role in arousal and reward mechanisms. Nicotine is most commonly used in the form of tobacco products like cigarettes or chewing tobacco; therefore, there is a tremendous interest in developing effective smoking cessation techniques. To date, people have used a variety of nicotine replacement therapies in addition to various psychotherapeutic options in an attempt to discontinue their use of tobacco products. In general, smoking cessation programs may be effective in the short term, but it is unclear whether these effects persist (Cropley, Theadom, Pravettoni, & Webb, 2008; Levitt, Shaw, Wong, & Kaczorowski, 2007; Smedslund, Fisher, Boles, & Lichtenstein, 2004).
Link to Learning
Try It
Opioids
An opioiopioidd is one of a category of drugs that includes heroin, morphine, methadone, and codeine. Opioids have analgesic properties; that is, they decrease pain. Humans have an endogenous opioid neurotransmitter system—the body makes small quantities of opioid compounds that bind to opioid receptors reducing pain and producing euphoria. Thus, opioid drugs, which mimic this endogenous painkilling mechanism, have an extremely high potential for abuse. Natural opioids, called opiates, are derivatives of opium, which is a naturally occurring compound found in the poppy plant. There are now several synthetic versions of opiate drugs (correctly called opioids) that have very potent painkilling effects, and they are often abused. For example, the National Institutes of Drug Abuse has sponsored research that suggests the misuse and abuse of the prescription pain killers hydrocodone and oxycodone are significant public health concerns (Maxwell, 2006). In 2013, the U.S. Food and Drug Administration recommended tighter controls on their medical use.

Aside from their utility as analgesic drugs, opioid-like compounds are often found in cough suppressants, anti-nausea, and anti-diarrhea medications. Given that withdrawal from a drug often involves an experience opposite to the effect of the drug, it should be no surprise that opioid withdrawal resembles a severe case of the flu. While opioid withdrawal can be extremely unpleasant, it is not life-threatening (Julien, 2005). Still, people experiencing opioid withdrawal may be given methadone to make withdrawal from the drug less difficult. Methadone is a synthetic opioid that is less euphorigenic than heroin and similar drugs. Methadone clinics help people who previously struggled with opioid addiction manage withdrawal symptoms through the use of methadone. Other drugs, including the opioid buprenorphine, have also been used to alleviate symptoms of opiate withdrawal.
Codeine is an opioid with relatively low potency. It is often prescribed for minor pain, and it is available over-the-counter in some other countries. Like all opioids, codeine does have abuse potential. In fact, abuse of prescription opioid medications is becoming a major concern worldwide (Aquina, Marques-Baptista, Bridgeman, & Merlin, 2009; Casati, Sedefov, & Pfeiffer-Gerschel, 2012).
Dig Deeper: The Opiod Epidemic
The opioid epidemic, or the opioid crisis, refers to the extensive overuse of opioid drugs, both from medical prescriptions and from illegal sources. The epidemic began slowly in the United States, beginning in the late 1990s, and led to a massive increase in opioid use in recent years, contributing to over 70,000 drug overdose deaths in the U.S. in 2018. Fentanyl alone, being 50 times stronger than heroin and 100 times stronger than morphine, was causing about 200 overdose deaths per day in 2017.[5]
Opioids are a diverse class of moderately strong, addictive, inexpensive painkillers prescribed by doctors. In the late 1990s, pharmaceutical companies reassured the medical community that patients would not become addicted to opioid pain relievers and healthcare providers began to prescribe them at greater rates. This led to widespread misuse of both prescription and non-prescription opioids before it became clear that these medications could indeed be highly addictive.
Though aggressive opioid prescription practices played the biggest role in creating the epidemic, the popularity of illegal substances such as potent heroin and illicit fentanyl have become an increasingly large factor. It has been suggested that decreased supply of prescription opioids caused by opioid prescribing reforms turned people who were already addicted to opioids towards illegal substances.[6]
In 2015, approximately 50% of drug overdoses were not the result of an opioid product from a prescription, though most abusers' first exposure had still been by lawful prescription.[7] By 2018, another study suggested that 75% of opioid abusers started their opioid use by taking drugs which had been obtained in a way other than by legitimate prescription.[8]
Those addicted to opioids, both legal and illegal, are increasingly young, white, and female, with 1.2 million women addicted compared to 0.9 million men in 2015. The populations of rural areas of the country have been the hardest hit. Teen abuse of opioids has been noticeably increasing since 2006, using prescription drugs more than any illicit drug except marijuana; more than cocaine, heroin, and methamphetamine combined. The crisis has also changed moral, social, and cultural resistance to street drug alternatives such as heroin.
Try It
Hallucinogens

A hallucinogen is one of a class of drugs that results in profound alterations in sensory and perceptual experiences (Figure 24). In some cases, users experience vivid visual hallucinations. Common hallucinogens include marijuana, psilocybin (shrooms), mescaline (peyote), and LSD. It is also common for these types of drugs to cause hallucinations of body sensations (e.g., feeling as if you are a giant) and a skewed perception of the passage of time.
As a group, hallucinogens are incredibly varied in terms of the neurotransmitter systems they affect. Mescaline and LSD are serotonin agonists, and PCP (angel dust) and ketamine (an animal anesthetic) act as antagonists of the NMDA glutamate receptor. In general, these drugs are not thought to possess the same sort of abuse potential as other classes of drugs discussed in this section.
Dig Deeper: Medical Marijuana
While the possession and use of marijuana is illegal in much of the United States, since January 2019, it is legal for recreational use in eleven states, and medical marijuana use is now legal in over half of the United States. Medical marijuana is marijuana that is prescribed by a doctor for the treatment of a health condition. For example, people who undergo chemotherapy will often be prescribed marijuana to stimulate their appetites and prevent excessive weight loss resulting from the side effects of chemotherapy treatment. Marijuana may also have some promise in the treatment of a variety of medical conditions (Mather, Rauwendaal, Moxham-Hall, & Wodak, 2013; Robson, 2014; Schicho & Storr, 2014).

While medical marijuana laws have been passed on a state-by-state basis, federal laws still classify this as an illicit substance, making conducting research on the potentially beneficial medicinal uses of marijuana problematic. There is quite a bit of controversy within the scientific community as to the extent to which marijuana might have medicinal benefits due to a lack of large-scale, controlled research (Bostwick, 2012). As a result, many scientists have urged the federal government to allow for relaxation of current marijuana laws and classifications in order to facilitate a more widespread study of the drug’s effects (Aggarwal et al., 2009; Bostwick, 2012; Kogan & Mechoulam, 2007).
Until recently, the United States Department of Justice routinely arrested people involved and seized marijuana used in medicinal settings. In the latter part of 2013, however, the United States Department of Justice issued statements indicating that they would not continue to challenge state medical marijuana laws. This shift in policy was likely a response to the scientific community’s recommendations and also a reflection changing public opinion regarding marijuana.
Try It
Summary of Psychoactive Drugs
Substance use disorder is defined in DSM-5 as a compulsive pattern of drug use despite negative consequences. Both physical and psychological dependence are important parts of this disorder. Alcohol, barbiturates, and benzodiazepines are central nervous system depressants that affect GABA neurotransmission. Cocaine, amphetamine, cathinones, and MDMA are all central nervous stimulants that agonize dopamine neurotransmission, while nicotine and caffeine affect acetylcholine and adenosine, respectively. Opiate drugs serve as powerful analgesics through their effects on the endogenous opioid neurotransmitter system, and hallucinogenic drugs cause pronounced changes in sensory and perceptual experiences. The hallucinogens are variable with regards to the specific neurotransmitter systems they affect.
Link to Learning
Try It
Hypnosis and Meditation
Our states of consciousness change as we move from wakefulness to sleep. We also alter our consciousness through the use of various psychoactive drugs. This final section will consider hypnotic and meditative states as additional examples of altered states of consciousness experienced by some individuals.
Hypnosis
Hypnosis is a state of extreme self-focus and attention in which minimal attention is given to external stimuli. In the therapeutic setting, a clinician often will use relaxation and suggestion in an attempt to alter the thoughts and perceptions of a patient. Hypnosis has also been used to draw out information believed to be buried deeply in someone’s memory. For individuals who are especially open to the power of suggestion, this can prove to be a very effective technique, and brain imaging studies have demonstrated that hypnotic states are associated with global changes in brain functioning (Del Casale et al., 2012; Guldenmund, Vanhaudenhuyse, Boly, Laureys, & Soddu, 2012).
Historically, hypnosis has been viewed with some suspicion because of its portrayal in popular media and entertainment (Figure 26). Therefore, it is important to make a distinction between hypnosis as an empirically based therapeutic approach versus as a form of entertainment. Contrary to popular belief, individuals undergoing hypnosis usually have clear memories of the hypnotic experience and are in control of their own behaviors. While hypnosis may be useful in enhancing memory or a skill, such enhancements are very modest in nature (Raz, 2011).

How exactly does a hypnotist bring a participant to a state of hypnosis? While there are variations, there are four parts that appear consistent in bringing people into the state of suggestibility associated with hypnosis (National Research Council, 1994). These components include:
The participant is guided to focus on one thing, such as the hypnotist’s words or a ticking watch. The participant is made comfortable and is directed to be relaxed and sleepy. The participant is told to be open to the process of hypnosis, trust the hypnotist and let go. The participant is encouraged to use his or her imagination.
These steps are conducive to being open to the heightened suggestibility of hypnosis.
People vary in terms of their ability to be hypnotized, but a review of available research suggests that most people are at least moderately hypnotizable (Kihlstrom, 2013). Hypnosis in conjunction with other techniques is used for a variety of therapeutic purposes and has shown to be at least somewhat effective for pain management, treatment of depression and anxiety, smoking cessation, and weight loss (Alladin, 2012; Elkins, Johnson, & Fisher, 2012; Golden, 2012; Montgomery, Schnur, & Kravits, 2012).
Some scientists are working to determine whether the power of suggestion can affect cognitive processes such as learning, with a view to using hypnosis in educational settings (Wark, 2011). Furthermore, there is some evidence that hypnosis can alter processes that were once thought to be automatic and outside the purview of voluntary control, such as reading (Lifshitz, Aubert Bonn, Fischer, Kashem, & Raz, 2013; Raz, Shapiro, Fan, & Posner, 2002). However, it should be noted that others have suggested that the automaticity of these processes remains intact (Augustinova & Ferrand, 2012).
How does hypnosis work? Two theories attempt to answer this question: One theory views hypnosis as dissociation and the other theory views it as the performance of a social role. According to the dissociation view, hypnosis is effectively a dissociated state of consciousness, much like our earlier example where you may drive to work, but you are only minimally aware of the process of driving because your attention is focused elsewhere. This theory is supported by Ernest Hilgard’s research into hypnosis and pain. In Hilgard’s experiments, he induced participants into a state of hypnosis, and placed their arms into ice water. Participants were told they would not feel pain, but they could press a button if they did; while they reported not feeling pain, they did, in fact, press the button, suggesting a dissociation of consciousness while in the hypnotic state (Hilgard & Hilgard, 1994).
Taking a different approach to explain hypnosis, the social-cognitive theory of hypnosis sees people in hypnotic states as performing the social role of a hypnotized person. As you will learn when you study social roles, people’s behavior can be shaped by their expectations of how they should act in a given situation. Some view a hypnotized person’s behavior not as an altered or dissociated state of consciousness, but as their fulfillment of the social expectations for that role.
Try It
Meditation
Meditation is the act of focusing on a single target (such as the breath or a repeated sound) to increase awareness of the moment. While hypnosis is generally achieved through the interaction of a therapist and the person being treated, an individual can perform meditation alone. Often, however, people wishing to learn to meditate receive some training in techniques to achieve a meditative state. A meditative state, as shown by EEG recordings of newly-practicing meditators, is not an altered state of consciousness per se; however, patterns of brain waves exhibited by expert meditators may represent a unique state of consciousness (Fell, Axmacher, & Haupt, 2010).
Although there are a number of different techniques in use, the central feature of all meditation is clearing the mind in order to achieve a state of relaxed awareness and focus (Chen et al., 2013; Lang et al., 2012). Mindfulness meditation has recently become popular. In the variation of meditation, the meditator’s attention is focused on some internal process or an external object (Zeidan, Grant, Brown, McHaffie, & Coghill, 2012).
Meditative techniques have their roots in religious practices (Figure 27), but their use has grown in popularity among practitioners of alternative medicine. Research indicates that meditation may help reduce blood pressure, and the American Heart Association suggests that meditation might be used in conjunction with more traditional treatments as a way to manage hypertension, although there is not sufficient data for a recommendation to be made (Brook et al., 2013). Like hypnosis, meditation also shows promise in stress management, sleep quality (Caldwell, Harrison, Adams, Quin, & Greeson, 2010), treatment of mood and anxiety disorders (Chen et al., 2013; Freeman et al., 2010; Vøllestad, Nielsen, & Nielsen, 2012), and pain management (Reiner, Tibi, & Lipsitz, 2013).

Link to Learning
Try It
Think It Over
- Under what circumstances would you be willing to consider hypnosis and/or meditation as a treatment option? What kind of information would you need before you made a decision to use these techniques?
Try It
States of Consciousness
Learning Objectives
In this chapter, you learned to:
- describe consciousness and biological rhythms
- describe what happens to the brain and body during sleep
- explain how drugs affect consciousness
Remember that psychology is the study of the mind and behavior. Consider how your behavior is affected by varying states of consciousness---what happens if you don't get enough sleep? How does your concentration and mood change? What happens to your conscious awareness when you take strong medications or drugs? In this module, you learned that varying states of consciousness, whether it be tiredness from jet lag, deep sleep, daydreaming, alcohol or drug use, hypnosis, or meditation, can all change physiological components in the mind as well as behavior. While we have control over some of these altered states, like meditation, there are sometimes variables outside of our control that lead to things like sleep disorders. Drug use often begins as a personal choice or something prescribed by a doctor, but many drugs have addictive qualities that make them hard to put down.
Substance abuse disorders can develop out of drug use, and those with drug addictions struggle with physical and psychological dependence on the drug. This is an especially important issue for us today because death by drug overdoses has been dramatically increasing over the past few years. Take a look at the interactive below to see the increasing prevalence of drug overdoses.
Link to Learning

As you read in the article above, in 2015 there were 52,000 American deaths from all drug overdoses. Two thirds of them, 33,000, were from opioids, compared to 16,000 in 2010 and 4,000 in 1999. Death from opioid drug overdoses were nearly equal to the number of deaths from car crashes, with deaths from heroin alone accounting for more deaths than from gun violence. In 2016, deaths from overdoses increased over the previous year by 26% in Connecticut, 35% in Delaware, 39% in Maine, and 62% in Maryland. Nearly half of all opioid overdose deaths involve a prescription opioid.
The governor of Maryland declared a State of Emergency in March 2017 to combat the epidemic and CDC director Thomas Frieden has said that "America is awash in opioids; urgent action is critical."
With this sudden, extreme increase in drug overdoses, psychologists and psychiatrists will continue to play an important role in researching, educating, and preventing substance abuse disorders. You can read more about what researchers are doing at the Addiction Connection or even find some practical tips on ways to prevent a drug overdose in this article from Psychology Today.
Chapter References (Click to expand)
Aggarwal, S. K., Carter, G. T., Sullivan, M. D., ZumBrunnen, C., Morrill, R., & Mayer, J. D. (2009). Medicinal use of cannabis in the United States: Historical perspectives, current trends, and future directions. Journal of Opioid Management, 5, 153–168.
Alhola, P. & Polo-Kantola, P. (2007). Sleep Deprivation: Impact on cognitive performance. Neuropsychiatric Disease and Treatment, 3, 553–557.
Alladin, A. (2012). Cognitive hypnotherapy for major depressive disorder. The American Journal of Clinical Hypnosis, 54, 275–293.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author.
Aquina, C. T., Marques-Baptista, A., Bridgeman, P., & Merlin, M. A. (2009). Oxycontin abuse and overdose. Postgraduate Medicine, 121, 163–167.
Arnulf, I. (2012). REM sleep behavior disorder: Motor manifestations and pathophysiology. Movement Disorders, 27, 677–689.
Augustinova, M., & Ferrand, L. (2012). Suggestion does not de-automatize word reading: Evidence from the semantically based Stroop task. Psychonomic Bulletin & Review, 19, 521–527.
Banks, S., & Dinges, D. F. (2007). Behavioral and physiological consequences of sleep restriction. Journal of Clinical Sleep Medicine, 3, 519–528.
Bartke, A., Sun, L. Y., & Longo, V. (2013). Somatotropic signaling: Trade-offs between growth, reproductive development, and longevity. Physiological Reviews, 93, 571–598.
Berkowitz, C. D. (2012). Sudden infant death syndrome, sudden unexpected infant death, and apparent life-threatening events. Advances in Pediatrics, 59, 183–208.
Berry, R. B., Kryger, M. H., & Massie, C. A. (2011). A novel nasal excitatory positive airway pressure (EPAP) device for the treatment of obstructive sleep apnea: A randomized controlled trial. Sleep, 34, 479–485.
Bixler, E. O., Kales, A., Soldatos, C. R., Kales, J. D., & Healey, S. (1979). Prevalence of sleep disorders in the Los Angeles metropolitan area. American Journal of Psychiatry, 136, 1257–1262.
Bostwick, J. M. (2012). Blurred boundaries: The therapeutics and politics of medical marijuana. Mayo Clinic Proceedings, 87, 172–186.
Brook, R. D., Appel, L. J., Rubenfire, M., Ogedegbe, G., Bisognano, J. D., Elliott, W. K., . . . Rajagopalan, S. (2013). Beyond medications and diet: Alternative approaches to lowering blood pressure: A scientific statement from the American Heart Association. Hypertension, 61, 1360–1383.
Broughton, R., Billings, R., Cartwright, R., Doucette, D., Edmeads, J., Edwardh, M., . . . Turrell, G. (1994). Homicidal somnambulism: A case report. Sleep, 17, 253–264.
Brown, L. K. (2012). Can sleep deprivation studies explain why human adults sleep? Current Opinion in Pulmonary Medicine, 18, 541–545.
Burgess, C. R., & Scammell, T. E. (2012). Narcolepsy: Neural mechanisms of sleepiness and cataplexy. Journal of Neuroscience, 32, 12305–12311.
Cai, D. J., Mednick, S. A., Harrison, E. M., Kanady, J. C., & Mednick, S. C. (2009). REM, not incubation, improves creativity by priming associative networks. Proceedings of the National Academy of Sciences, USA, 106, 10130–10134.
Caldwell, K., Harrison, M., Adams, M., Quin, R. H., & Greeson, J. (2010). Developing mindfulness in college students through movement based courses: Effects on self-regulatory self-efficacy, mood, stress, and sleep quality. Journal of American College Health, 58, 433–442.
Capellini, I., Barton, R. A., McNamara, P., Preston, B. T., & Nunn, C. L. (2008). Phylogenetic analysis of the ecology and evolution of mammalian sleep. Evolution, 62, 1764–1776.
Cartwright, R. (2004). Sleepwalking violence: A sleep disorder, a legal dilemma, and a psychological challenge. American Journal of Psychiatry, 161, 1149–1158.
Cartwright, R., Agargun, M. Y., Kirkby, J., & Friedman, J. K. (2006). Relation of dreams to waking concerns. Psychiatry Research, 141, 261–270.
Casati, A., Sedefov, R., & Pfeiffer-Gerschel, T. (2012). Misuse of medications in the European Union: A systematic review of the literature. European Addiction Research, 18, 228–245.
Chen, K. W., Berger, C. C., Manheimer, E., Forde, D., Magidson, J., Dachman, L., & Lejuez, C. W. (2013). Meditative therapies for reducing anxiety: A systematic review and meta-analysis of randomized controlled trials. Depression and Anxiety, 29, 545–562.
Chokroverty, S. (2010). Overview of sleep & sleep disorders. Indian Journal of Medical Research, 131, 126–140.
Christensen, A., Bentley, G. E., Cabrera, R., Ortega, H. H., Perfito, N., Wu, T. J., & Micevych, P. (2012). Hormonal regulation of female reproduction. Hormone and Metabolic Research, 44, 587–591.
CNN. (1999, June 25). ‘Sleepwalker’ convicted of murder. Retrieved from http://www.cnn.com/US/9906/25/sleepwalker.01/
Cropley, M., Theadom, A., Pravettoni, G., & Webb, G. (2008). The effectiveness of smoking cessation interventions prior to surgery: A systematic review. Nicotine and Tobacco Research, 10, 407–412.
De la Herrán-Arita, A. K., & Drucker-Colín, R. (2012). Models for narcolepsy with cataplexy drug discovery. Expert Opinion on Drug Discovery, 7, 155–164.
Del Casale, A., Ferracuti, S., Rapinesi, C., Serata, D., Sani, G., Savoja, V., . . . Girardi, P. (2012). Neurocognition under hypnosis: Findings from recent functional neuroimaging studies. International Journal of Clinical and Experimental Hypnosis, 60, 286–317.
Elkins, G., Johnson, A., & Fisher, W. (2012). Cognitive hypnotherapy for pain management. The American Journal of Clinical Hypnosis, 54, 294–310.
Ellenbogen, J. M., Hu, P. T., Payne, J. D., Titone, D., & Walker, M. P. (2007). Human relational memory requires time and sleep. Proceedings of the National Academy of Sciences, USA, 104, 7723–7728.
Fell, J., Axmacher, N., & Haupt, S. (2010). From alpha to gamma: Electrophysiological correlates meditation-related states of consciousness. Medical Hypotheses, 75, 218–224.
Fenn, K. M., Nusbaum, H. C., & Margoliash, D. (2003). Consolidation during sleep of perceptual learning of spoken language. Nature, 425, 614–616.
Ferini-Strambi, L. (2011). Does idiopathic REM sleep behavior disorder (iRBD) really exist? What are the potential markers of neurodegeneration in iRBD [Supplemental material]? Sleep Medicine, 12(2 Suppl.), S43–S49.
Fiorentini, A., Volonteri, L.S., Dragogna, F., Rovera, C., Maffini, M., Mauri, M. C., & Altamura, C. A. (2011). Substance-induced psychoses: A critical review of the literature. Current Drug Abuse Reviews, 4, 228–240.
Fogel, S. M., & Smith, C. T. (2011). The function of the sleep spindle: A physiological index of intelligence and a mechanism for sleep-dependent memory consolidation. Neuroscience and Biobehavioral Reviews, 35, 1154–1165.
Frank, M. G. (2006). The mystery of sleep function: Current perspectives and future directions. Reviews in the Neurosciences, 17, 375–392.
Freeman, M. P., Fava, M., Lake, J., Trivedi, M. H., Wisner, K. L., & Mischoulon, D. (2010). Complementary and alternative medicine in major depressive disorder: The American Psychiatric Association task force report. The Journal of Clinical Psychiatry, 71, 669–681.
Giedke, H., & Schwärzler, F. (2002). Therapeutic use of sleep deprivation in depression. Sleep Medicine Reviews, 6, 361–377.
Gold, D. R., Rogacz, S. R., Bock, N., Tosteson, T. D., Baum, T. M., Speizer, F. M., & Czeisler, C. A. (1992). Rotating shift work, sleep, and accidents related to sleepiness in hospital nurses. American Journal of Public Health, 82, 1011–1014.
Golden, W. L. (2012). Cognitive hypnotherapy for anxiety disorders. The American Journal of Clinical Hypnosis, 54, 263–274.
Gómez, R. L., Bootzin, R. R., & Nadel, L. (2006). Naps promote abstraction in language-learning infants. Psychological Science, 17, 670–674.
Guilleminault, C., Kirisoglu, C., Bao, G., Arias, V., Chan, A., & Li, K. K. (2005). Adult chronic sleepwalking and its treatment based on polysomnography. Brain, 128, 1062–1069.
Gujar, N., Yoo, S., Hu, P., & Walker, M. P. (2011). Sleep deprivation amplifies reactivity of brain reward networks, biasing the appraisal of positive emotional experiences. The Journal of Neuroscience, 31, 4466–4474.
Guldenmund, P., Vanhaudenhuyse, A., Boly, M., Laureys, S., & Soddu, A. (2012). A default mode of brain function in altered states of consciousness. Archives Italiennes de Biologie, 150, 107–121.
Halász, P. (1993). Arousals without awakening—Dynamic aspect of sleep. Physiology and Behavior, 54, 795–802.
Han, F. (2012). Sleepiness that cannot be overcome: Narcolepsy and cataplexy. Respirology, 17, 1157–1165.
Hardeland, R., Pandi-Perumal, S. R., & Cardinali, D. P. (2006). Melatonin. International Journal of Biochemistry & Cell Biology, 38, 313–316.
Haasen, C., & Krausz, M. (2001). Myths versus experience with respect to cocaine and crack: Learning from the US experience. European Addiction Research, 7, 159–160.
Henry, D., & Rosenthal, L. (2013). “Listening for his breath:” The significance of gender and partner reporting on the diagnosis, management, and treatment of obstructive sleep apnea. Social Science & Medicine, 79, 48–56.
Hicks, R. A., Fernandez, C., & Pelligrini, R. J. (2001). The changing sleep habits of university students: An update. Perceptual and Motor Skills, 93, 648.
Hicks, R. A., Johnson, C., & Pelligrini, R. J. (1992). Changes in the self-reported consistency of normal habitual sleep duration of college students (1978 and 1992). Perceptual and Motor Skills, 75, 1168–1170.
Hilgard, E. R., & Hilgard, J. R. (1994). Hypnosis in the Relief of Pain. New York: Brunner/Mazel.
Hishikawa, Y., & Shimizu, T. (1995). Physiology of REM sleep, cataplexy, and sleep paralysis. Advances in Neurology, 67, 245–271.
Herman, A., & Herman, A. P. (2013). Caffeine’s mechanism of action and its cosmetic use. Skin Pharmacology and Physiology, 26, 8–14.
Hobson, J. A. (2009). REM sleep and dreaming: Towards a theory of protoconsciousness. Nature Reviews Neuroscience, 10, 803–814.
Horikawa,T., Tamaki, M., Miyawaki, Y. & Kamitani, Y. (2013). Neural Decoding of Visual Imagery During Sleep. Science, 340(6132), 639–642. doi:10.1126/science.1234330
Hossain, J. L., & Shapiro, C. M. (2002). The prevalence, cost implications, and management of sleep disorders: An overview. Sleep and Breathing, 6, 85–102.
Huang, L. B., Tsai, M. C., Chen, C. Y., & Hsu, S. C. (2013). The effectiveness of light/dark exposure to treat insomnia in female nurses undertaking shift work during the evening/night shift. Journal of Clinical Sleep Medicine, 9, 641–646.
Huber, R., Ghilardi, M. F., Massimini, M., & Tononi, G. (2004). Local sleep and learning. Nature, 430, 78–81.
Jayanthi, L. D., & Ramamoorthy, S. (2005). Regulation of monoamine transporters: Influence of psychostimulants and therapeutic antidepressants. The AAPS Journal, 7, E728–738.
Julien, R. M. (2005). Opioid analgesics. In A primer of drug action: A comprehensive guide to the actions, uses, and side effects of psychoactive drugs (pp. 461–500). Portland, OR: Worth.
Kihlstrom, J. F. (2013). Neuro-hypnotism: Prospects for hypnosis and neuroscience. Cortex, 49, 365–374.
Klein, D. C., Moore, R. Y., & Reppert, S. M. (Eds.). (1991). Suprachiasmatic nucleus: The mind’s clock. New York, NY: Oxford University Press.
Kogan, N. M., & Mechoulam, R. (2007). Cannabinoids in health and disease. Dialogues in Clinical Neuroscience, 9, 413–430.
Kromann, C. B., & Nielson, C. T. (2012). A case of cola dependency in a woman with recurrent depression. BMC Research Notes, 5, 692.
Lang, A. J., Strauss, J. L., Bomeya, J., Bormann, J. E., Hickman, S. D., Good, R. C., & Essex, M. (2012). The theoretical and empirical basis for meditation as an intervention for PTSD. Behavior Modification, 36, 759–786.
LaBerge, S. (1990). Lucid dreaming: Psychophysiological studies of consciousness during REM sleep. In R. R. Bootzen, J. F. Kihlstrom, & D. L. Schacter (Eds.), Sleep and cognition (pp. 109–126). Washington, DC: American Psychological Association.
Lesku, J. A., Roth, T. C., 2nd, Amlaner, C. J., & Lima, S. L. (2006). A phylogenetic analysis of sleep architecture in mammals: The integration of anatomy, physiology, and ecology. The American Naturalist, 168, 441–453.
Levitt, C., Shaw, E., Wong, S., & Kaczorowski, J. (2007). Systematic review of the literature on postpartum care: Effectiveness of interventions for smoking relapse prevention, cessation, and reduction in postpartum women. Birth, 34, 341–347.
Lifshitz, M., Aubert Bonn, N., Fischer, A., Kashem, I. F., & Raz, A. (2013). Using suggestion to modulate automatic processes: From Stroop to McGurk and beyond. Cortex, 49, 463–473.
Luppi, P. H., Clément, O., Sapin, E., Gervasoni, D., Peyron, C., Léger, L., . . . Fort, P. (2011). The neuronal network responsible for paradoxical sleep and its dysfunctions causing narcolepsy and rapid eye movement (REM) behavior disorder. Sleep Medicine Reviews, 15, 153–163.
Mage, D. T., & Donner, M. (2006). Female resistance to hypoxia: Does it explain the sex difference in mortality rates? Journal of Women’s Health, 15, 786–794.
Mahowald, M. W., & Schenck, C. H. (2000). Diagnosis and management of parasomnias. Clinical Cornerstone, 2, 48–54.
Mahowald, M. W., Schenck, C. H., & Cramer Bornemann, M. A. (2005). Sleep-related violence. Current Neurology and Neuroscience Reports, 5, 153–158.
Mayo Clinic. (n.d.). Sleep terrors (night terrors). Retrieved from http://www.mayoclinic.org/diseases-conditions/night-terrors/basics/treatment/con-20032552
Mather, L. E., Rauwendaal, E. R., Moxham-Hall, V. L., & Wodak, A. D. (2013). (Re)introducing medical cannabis. The Medical Journal of Australia, 199, 759–761.
Maxwell, J. C. (2006). Trends in the abuse of prescription drugs. Gulf Coast Addiction Technology Transfer Center. Retrieved from http://asi.nattc.org/userfiles/file/GulfCoast/PrescriptionTrends_Web.pdf
McCarty, D. E. (2010). A case of narcolepsy with strictly unilateral cataplexy. Journal of Clinical Sleep Medicine, 15, 75–76.
McDaid, C., Durée, K. H., Griffin, S. C., Weatherly, H. L., Stradling, J. R., Davies, R. J., . . . Westwood, M. E. (2009). A systematic review of continuous positive airway pressure for obstructive sleep apnoea-hypopnoea syndrome. Sleep Medicine Reviews, 13, 427–436.
McKim, W. A., & Hancock, S. D. (2013). Drugs and behavior: An introduction to behavioral pharmacology, 7th edition. Boston, MA: Pearson.
Mignot, E. J. M. (2012). A practical guide to the therapy of narcolepsy and hypersomnia syndromes. Neurotherapeutics, 9, 739–752.
Miller, N. L., Shattuck, L. G., & Matsangas, P. (2010). Longitudinal study of sleep patterns of United States Military Academy cadets. Sleep, 33, 1623–1631.
Mitchell, E. A. (2009). SIDS: Past, present and future. Acta Paediatrica, 98, 1712–1719.
Montgomery, G. H., Schnur, J. B., & Kravits, K. (2012). Hypnosis for cancer care: Over 200 years young. CA: A Cancer Journal for Clinicians, 63, 31–44.
National Institutes of Health. (n.d.). Information about sleep. Retrieved from http://science.education.nih.gov/supplements/nih3/sleep/guide/info-sleep.htm
National Research Council. (1994). Learning, remembering, believing: Enhancing human performance. Washington, DC: The National Academies Press.
National Sleep Foundation. (n.d.). How much sleep do we really need? Retrieved from http://sleepfoundation.org/how-sleep-works/how-much-sleep-do-we-really-need
Ohayon, M. M. (1997). Prevalence of DSM-IV diagnostic criteria of insomnia: Distinguishing insomnia related to mental disorders from sleep disorders. Journal of Psychiatric Research, 31, 333–346.
Ohayon, M. M. (2002). Epidemiology of insomnia: What we know and what we still need to learn. Sleep Medicine Reviews, 6, 97–111.
Ohayon, M. M., Carskadon, M. A., Guilleminault, C., & Vitiello, M. V. (2004). Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep, 27, 1255–1273.
Ohayon, M. M., & Roth, T. (2002). Prevalence of restless legs syndrome and periodic limb movement disorder in the general population. Journal of Psychosomatic Research, 53, 547–554.
Poe, G. R., Walsh, C. M., & Bjorness, T. E. (2010). Cognitive neuroscience of sleep. Progress in Brain Research, 185, 1–19.
Porkka-Heiskanen, T. (2011). Methylxanthines and sleep. Handbook of Experimental Pharmacology, 200, 331–348.
Presser, H. B. (1995). Job, family, and gender: Determinants of nonstandard work schedules among employed Americans in 1991. Demography, 32, 577–598.
Pressman, M. R. (2007). Disorders of arousal from sleep and violent behavior: The role of physical contact and proximity. Sleep, 30, 1039–1047.
Provini, F., Tinuper, P., Bisulli, F., & Lagaresi, E. (2011). Arousal disorders [Supplemental material]. Sleep Medicine, 12(2 Suppl.), S22–S26.
Rattenborg, N. C., Lesku, J. A., Martinez-Gonzalez, D., & Lima, S. L. (2007). The non-trivial functions of sleep. Sleep Medicine Reviews, 11, 405–409.
Raz, A. (2011). Hypnosis: A twilight zone of the top-down variety: Few have never heard of hypnosis but most know little about the potential of this mind-body regulation technique for advancing science. Trends in Cognitive Sciences, 15, 555–557.
Raz, A., Shapiro, T., Fan, J., & Posner, M. I. (2002). Hypnotic suggestion and the modulation of Stroop interference. Archives of General Psychiatry, 59, 1151–1161.
Reiner, K., Tibi, L., & Lipsitz, J. D. (2013). Do mindfulness-based interventions reduce pain intensity? A critical review of the literature. Pain Medicine, 14, 230–242.
Restless Legs Syndrome Foundation. (n.d.). Restless legs syndrome: Causes, diagnosis, and treatment for the patient living with Restless legs syndrome (RSL). Retrieved from www.rls.org
Rial, R. V., Nicolau, M. C., Gamundí, A., Akaârir, M., Aparicio, S., Garau, C., . . . Esteban, S. (2007). The trivial function of sleep. Sleep Medicine Reviews, 11, 311–325.
Riemann, D., Berger, M., & Volderholzer, U. (2001). Sleep and depression—Results from psychobiological studies: An overview. Biological Psychology, 57, 67–103.
Reinerman, C. (2007, October 14). 5 myths about that demon crack. Washington Post. Retrieved from http://www.washingtonpost.com/wp-dyn/content/article/2007/10/09/AR2007100900751.html
Reissig, C. J., Strain, E. C., & Griffiths, R. R. (2009). Caffeinated energy drinks—A growing problem. Drug and Alcohol Dependence, 99, 1–10.
Robson, P. J. (2014). Therapeutic potential of cannabinoid medicines. Drug Testing and Analysis, 6, 24–30.
Roth, T. (2007). Insomnia: Definition, prevalence, etiology, and consequences [Supplemental material]. Journal of Clinical Sleep Medicine, 3(5 Suppl.), S7–S10.
Rothman, R. B., Blough, B. E., & Baumann, M. H. (2007). Dual dopamine/serotonin releasers as potential medications for stimulant and alcohol addictions. The AAPS Journal, 9, E1–10.
Sánchez-de-la-Torre, M., Campos-Rodriguez, F., & Barbé, F. (2012). Obstructive sleep apnoea and cardiovascular disease. The Lancet Respiratory Medicine, 1, 31–72.
Savard, J., Simard, S., Ivers, H., & Morin, C. M. (2005). Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part I: Sleep and psychological effects. Journal of Clinical Oncology, 23, 6083–6096.
Schicho, R., & Storr, M. (2014). Cannabis finds its way into treatment of Crohn’s disease. Pharmacology, 93, 1–3.
Shukla, R. K, Crump, J. L., & Chrisco, E. S. (2012). An evolving problem: Methamphetamine production and trafficking in the United States. International Journal of Drug Policy, 23, 426–435.
Siegel, J. M. (2008). Do all animals sleep? Trends in Neuroscience, 31, 208–213.
Siegel, J. M. (2001). The REM sleep-memory consolidation hypothesis. Science, 294, 1058–1063.
Singh, G. K., & Siahpush, M. (2006). Widening socioeconomic inequalities in US life expectancy, 1980–2000. International Journal of Epidemiology, 35, 969–979.
Smedslund, G., Fisher, K. J., Boles, S. M., & Lichtenstein, E. (2004). The effectiveness of workplace smoking cessation programmes: A meta-analysis of recent studies. Tobacco Control, 13, 197–204.
Sofikitis, N., Giotitsas, N., Tsounapi, P., Baltogiannis, D., Giannakis, D., & Pardalidis, N. (2008). Hormonal regulation of spermatogenesis and spermiogenesis. Journal of Steroid Biochemistry and Molecular Biology, 109, 323–330.
Steriade, M., & Amzica, F. (1998). Slow sleep oscillation, rhythmic K-complexes, and their paroxysmal developments [Supplemental material]. Journal of Sleep Research, 7(1 Suppl.), 30–35.
Stickgold, R. (2005). Sleep-dependent memory consolidation. Nature, 437, 1272–1278.
Stone, K. C., Taylor, D. J., McCrae, C. S., Kalsekar, A., & Lichstein, K. L. (2008). Nonrestorative sleep. Sleep Medicine Reviews, 12, 275–288.
Suchecki, D., Tiba, P. A., & Machado, R. B. (2012). REM sleep rebound as an adaptive response to stressful situations. Frontiers in Neuroscience, 3. doi: 10.3389/fneur.2012.00041
Task Force on Sudden Infant Death Syndrome. (2011). SIDS and other sleep-related infant deaths: Expansion of recommendations for a safe infant sleeping environment. Pediatrics, 128, 1030–1039.
Taillard, J., Philip, P., Coste, O., Sagaspe, P., & Bioulac, B. (2003). The circadian and homeostatic modulation of sleep pressure during wakefulness differs between morning and evening chronotypes. Journal of Sleep Research, 12, 275–282.
Thach, B. T. (2005). The role of respiratory control disorders in SIDS. Respiratory Physiology & Neurobiology, 149, 343–353.
U.S. Food and Drug Administration. (2013, October 24). Statement on Proposed Hydrocodone Reclassification from Janet Woodcock, M.D., Director, Center for Drug Evaluation and Research. Retrieved from http://www.fda.gov/drugs/drugsafety/ucm372089.htm
Vogel, G. W. (1975). A review of REM sleep deprivation. Archives of General Psychiatry, 32, 749–761.
Vøllestad, J., Nielsen, M. B., & Nielsen, G. H. (2012). Mindfulness- and acceptance-based interventions for anxiety disorders: A systematic review and meta-analysis. The British Journal of Clinical Psychology, 51, 239–260.
Wagner, U., Gais, S., & Born, J. (2001). Emotional memory formation is enhanced across sleep intervals with high amounts of rapid eye movement sleep. Learning & Memory, 8, 112–119.
Wagner, U., Gais, S., Haider, H., Verleger, R., & Born, J. (2004). Sleep improves insight. Nature, 427, 352–355.
Walker, M. P. (2009). The role of sleep in cognition and emotion. Annals of the New York Academy of Sciences, 1156, 168–197.
Wark, D. M. (2011). Traditional and alert hypnosis for education: A literature review. The American Journal of Clinical Hypnosis, 54(2), 96–106.
Waterhouse. J., Fukuda, Y., & Morita, T. (2012). Daily rhythms of the sleep-wake cycle [Special issue]. Journal of Physiological Anthropology, 31(5). doi:10.1186/1880-6805-31-5
Welsh, D. K. Takahashi, J. S., & Kay, S. A. (2010). Suprachiasmatic nucleus: Cell autonomy and network properties. Annual Review of Physiology, 72, 551–577.
West, S., Boughton, M., & Byrnes, M. (2009). Juggling multiple temporalities: The shift work story of mid-life nurses. Journal of Nursing Management, 17, 110–119.
White, D. P. (2005). Pathogenesis of obstructive and central sleep apnea. American Journal of Respiratory and Critical Care Medicine, 172, 1363–1370.
Williams, J., Roth, A., Vatthauer, K., & McCrae, C. S. (2013). Cognitive behavioral treatment of insomnia. Chest, 143, 554–565.
Williamson, A. M., & Feyer, A. M. (2000). Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occupational and Environmental Medicine, 57, 649–655.
Wolt, B. J., Ganetsky, M., & Babu, K. M. (2012). Toxicity of energy drinks. Current Opinion in Pediatrics, 24, 243–251.
Zangini, S., Calandra-Buonaura, G., Grimaldi, D., & Cortelli, P. (2011). REM behaviour disorder and neurodegenerative diseases [Supplemental material]. Sleep Medicine, 12(2 Suppl.), S54–S58.
Zeidan, F., Grant, J. A., Brown, C. A., McHaffie, J. G., & Coghill, R. C. (2012). Mindfulness meditation-related pain relief: Evidence for unique brain mechanisms in the regulation of pain. Neuroscience Letters, 520, 165–173.
Licenses and Attributions (Click to expand)
CC licensed content, Original
- States of Consciousness. Authored by: Karenna Malavanti Provided by: PressBooks. License: CC BY-NC-SA: Attribution-NonCommercial-ShareAlike
CC licensed content, Shared previously
- Why It Matters: States of Consciousness. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY: Attribution Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/introduction-13/
- Introduction to States of Consciousness. Authored by: OpenStax College. License: CC BY: Attribution. License Terms: Download for free at https://openstax.org/books/psychology-2e/pages/1-introduction. Located at: https://openstax.org/books/psychology-2e/pages/4-introduction.
- Introduction to Consciousness and Rhythms. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY-SA: Attribution-ShareAlike Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/outcome-consciousness/
- What is Consciousness?. Authored by: OpenStax College. License: CC BY: Attribution. License Terms: Download for free at https://openstax.org/books/psychology-2e/pages/1-introduction Located at: https://openstax.org/books/psychology-2e/pages/4-1-what-is-consciousness.
- Zeitgeber. Provided by: Wikipedia. License: CC BY-SA: Attribution-ShareAlike. Located at: https://en.wikipedia.org/wiki/Zeitgeber.
- Chronotype. Provided by: Wikipedia. License: CC BY-SA: Attribution-ShareAlike. Located at: https://en.wikipedia.org/wiki/Chronotype.
- Psychology in Real Life: Blindsight. Authored by: Patrick Carroll for Lumen Learning. Provided by: Lumen Learning. License: CC BY-SA: Attribution-ShareAlike Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/psych-in-real-life-consciousness-and-blindsight/
- Visual pathways image. Provided by: Wikimedia. License: CC BY-SA: Attribution-ShareAlike. Located at: https://commons.wikimedia.org/wiki/File:Human_visual_pathway.svg.
- College student in the park. Authored by: CollegeDegrees360. License: CC BY-SA: Attribution-ShareAlike. Located at: https://www.flickr.com/photos/83633410@N07/7658074952.
- When Biological Clocks Get Disrupted. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY: Attribution-Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/reading-sleep-disruptions/
- Introduction to Sleep and Dreams. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY-SA: Attribution-ShareAlike Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/outcome-sleep-and-dreams/
- Sleep and Why We Sleep. Authored by: OpenStax College. License: CC BY: Attribution. License Terms: Download for free at https://openstax.org/books/psychology-2e/pages/1-introduction. Located at: https://openstax.org/books/psychology-2e/pages/4-2-sleep-and-why-we-sleep.
- Image of sleeping girl. Authored by: College Degrees 360. Provided by: Flickr. License: CC BY-SA: Attribution-ShareAlike. Located at: https://www.flickr.com/photos/83633410@N07/7658254172.
- Sleep and Why We Sleep. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY: Attribution Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/sleep-and-why-we-sleep/
- Stages of Sleep. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY-SA: Attribution-ShareAlike Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/stages-of-sleep/
- EEG and Sleep stages images. Authored by: Kim Louie for Lumen Learning. License: CC BY: Attribution
- Stages of Sleep. Authored by: OpenStax College. License: CC BY: Attribution. License Terms: Download for free at https://openstax.org/books/psychology-2e/pages/1-introduction. Located at: https://openstax.org/books/psychology-2e/pages/4-3-stages-of-sleep.
- Dreams and Dreaming. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY-SA: Attribution-ShareAlike Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/reading-dreams/
- The Nature and Meaning of Dreams. Provided by: Boundless. License: CC BY-SA: Attribution-ShareAlike. Located at: https://www.boundless.com/psychology/textbooks/boundless-psychology-textbook/states-of-consciousness-6/sleep-and-dreaming-42/the-nature-and-meaning-of-dreams-184-12719/.
- Sleeping woman. Authored by: Craig Adderley. Provided by: Pexels. License: CC0 No Rights Reserved. Located at: https://www.pexels.com/photo/woman-sleeping-1497855/.
- Sleep Problems and Disorders. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY-SA: Attribution-ShareAlike Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/sleep-problems-and-disorders/
- Sleep Problems and Disorders. Authored by: OpenStax College. License: CC BY: Attribution. License Terms: Download for free at https://openstax.org/books/psychology-2e/pages/1-introduction. Located at: https://openstax.org/books/psychology-2e/pages/4-3-stages-of-sleep.
- Introduction to Drugs and Other States of Consciousness. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY-SA: Attribution-ShareAlike Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/outcome-drugs-and-other-states-of-consciousness/
- Substance Use and Abuse. Authored by: OpenStax College. License: CC BY: Attribution. License Terms: Download for free at https://openstax.org/books/psychology-2e/pages/1-introduction. Located at: https://openstax.org/books/psychology-2e/pages/4-5-substance-use-and-abuse.
- Mandelbrot Islands of Consciousness image. Authored by: David R. Ingham. Provided by: Wikipedia. License: CC BY-SA: Attribution-ShareAlike. Located at: https://commons.wikimedia.org/wiki/File:Mandelbrot_Islands_of_Consciousness.jpg.
- Psychoactive Drugs and Addiction. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY: Attribution Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/reading-psychoactive-drugs/
- Alcohol and Other Depressants. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY-SA: Attribution-ShareAlike Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/reading-alcohol-and-other-depressants/
- Blood alcohol content. Authored by: Wikipedia. License: CC BY-SA: Attribution-ShareAlike. Located at: https://en.wikipedia.org/wiki/Blood_alcohol_content.
- Stimulants. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY: Attribution Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/reading-stimulants/
- Opioids. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY-SA: Attribution-ShareAlike Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/reading-opiods/
- Opioid Epidemic in the United States. Provided by: Wikipedia. License: CC BY-SA: Attribution-ShareAlike. Located at: https://en.wikipedia.org/wiki/Opioid_epidemic_in_the_United_States.
- Hallucinogens. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY: Attribution Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/reading-hallucinogens/
- Drugs interactive. Authored by: Jessica Traylor for Lumen Learning. Provided by: Lumen Learning. License: CC BY: Attribution
- Hypnosis and Meditation. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY: Attribution Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/other-states-of-consciousness/
- Other States of Consciousness. Authored by: OpenStax College. License: CC BY: Attribution. License Terms: Download for free at https://openstax.org/books/psychology-2e/pages/1-introduction. Located at: https://openstax.org/books/psychology-2e/pages/4-6-other-states-of-consciousness.
- Putting It Together: States of Consciousness. Authored by: Lumen Learning Provided by: Lumen Learning. License: CC BY-SA: Attribution-ShareAlike Located at: https://pressbooks.online.ucf.edu/lumenpsychology/chapter/putting-it-together-states-of-consciousness/
- Opioid Epidemic. Provided by: Wikipedia. License: CC BY-SA: Attribution-ShareAlike. Located at: https://en.wikipedia.org/wiki/Opioid_epidemic.
- Generic temazepam 10 mg tablets. Provided by: Wikipedia. License: CC BY-SA: Attribution-ShareAlike. Located at: https://en.wikipedia.org/wiki/Temazepam#/media/File:Temazepam_10mg_tablets-1.jpg.
All Rights Reserved Content
- Reprogramming Our Circadian Rhythms for the Modern World. Authored by: Big Think. License: Other. License Terms: Standard YouTube License. Located at: https://www.youtube.com/watch?v=rtCQ9jzC-Ek.
- TN Blindsight. Authored by: CANlabTilburg. License: Other. License Terms: Standard YouTube License. Located at: https://www.youtube.com/watch?v=ACkxe_5Ubq8.
- Part 3 - Phantoms In The Brain (Episode 1). Authored by: LennyBound. License: Other. License Terms: Standard YouTube License. Located at: https://www.youtube.com/watch?v=ny5qMKTcURE.
- What would happen if you didnt sleep? - Claudia Aguirre. Authored by: Ted-Ed. License: Other. License Terms: Standard YouTube License. Located at: https://www.youtube.com/watch?v=dqONk48l5vY.
- The Connection between Memory and Sleep - Science Nation. Authored by: National Science Foundation. License: Other. License Terms: Standard YouTube License. Located at: https://www.youtube.com/watch?v=ObuaXhtKbVY.
- To Sleep, Perchance to Dream - Crash Course Psychology #9. Provided by: CrashCourse. License: Other. License Terms: Standard YouTube License. Located at: https://www.youtube.com/watch?v=rMHus-0wFSo.
- Altered States - Crash Course Psychology #10. Provided by: CrashCourse. License: Other. License Terms: Standard YouTube License. Located at: https://youtu.be/9PW1fwKjo-Y?list=PL8dPuuaLjXtOPRKzVLY0jJY-uHOH9KVU6.
Public domain content
- Representation of consciousnes from the seventeenth century Authored by: Robert Fludd. Provided by: Wikipedia. License: Public Domain: No Known Copyright. Located at: https://en.wikipedia.org/wiki/Consciousness#/media/File:RobertFuddBewusstsein17Jh.png.
- Circadian rhythms. Provided by: National Institute of General Medical Science. License: Public Domain: No Known Copyright. Located at: https://www.nigms.nih.gov/education/pages/factsheet_circadianrhythms.aspx.
- What is the U.S. Opioid Epidemic?. Provided by: U.S. Department of Health and Human Services. License: Public Domain: No Known Copyright. Located at: https://www.hhs.gov/opioids/about-the-epidemic/index.html.
- Source: http://marketingland.com/wp-content/ml-loads/2014/09/iceberg-ss-1920.jpg ↵
- A recent literature review of evidence for the existence of the pathways to the cerebral cortex: Rabbo, F. A., Koch, G., Lefevre, C., & Seizeur, R. (2015). Direct geniculo-extrastriate pathways: A review of the literature. Surgical and Radiologic Anatomy, 37(8), 891-899. ↵
- See Consciousness Lost and Found: A Neuropsychological Exploration by Larry Weiskrantz (1997, Oxford University Press). Dr. Weiskrantz is one of the scientists who first described blindsight and studied people with the condition. ↵
- The physics of electromagnetism is fascinating, but we will spare you the details here. You may have studied it in some other class, and there are many readable online sources (e.g., Wikipedia). TMS is a great example of the convergence of technology and psychology that is the basis of modern neuroscience. ↵
- Fentanyl As A Dark Web Profit Center, From Chinese Labs To U.S. Streets", KUAR, NPR Radio News, Sept. 4, 2019 ↵
- Prescription Opioid Data". Centers for Disease Control and Prevention (CDC). Retrieved November 2, 2018. ↵
- Shipton EA, Shipton EE, Shipton AJ (June 2018). "A Review of the Opioid Epidemic: What Do We Do About It?". Pain and Therapy. 7 (1): 23–36. ↵
- Pergolizzi JV, LeQuang JA, Taylor R, Raffa RB (January 2018). "Going beyond prescription pain relievers to understand the opioid epidemic: the role of illicit fentanyl, new psychoactive substances, and street heroin". Postgraduate Medicine. 130 (1): 1–8. ↵
awareness of internal and external stimuli
state marked by relatively low levels of physical activity and reduced sensory awareness that is distinct from periods of rest that occur during wakefulness
characterized by high levels of sensory awareness, thought, and behavior
internal cycle of biological activity
biological rhythm that occurs over approximately 24 hours
state of equilibrium—biological conditions, such as body temperature, are maintained at optimal levels
area of the hypothalamus in which the body’s biological clock is located
collection of symptoms brought on by travel from one time zone to another that results from the mismatch between our internal circadian cycles and our environment
consistent difficulty in falling or staying asleep for at least three nights a week over a month’s time
work schedule that changes from early to late on a daily or weekly basis
result of insufficient sleep on a chronic basis
study that combines the results of several related studies
sleep-deprived individuals will experience shorter sleep latencies during subsequent opportunities for sleep
discipline that studies how universal patterns of behavior and cognitive processes have evolved over time as a result of natural selection
period of sleep characterized by brain waves very similar to those during wakefulness and by darting movements of the eyes under closed eyelids
type of brain wave characteristic during wakefulness, which has a very low amplitude and a frequency of 13–30 Hz
period of sleep outside periods of rapid eye movement (REM) sleep
type of rbrain wave characteristic during the early part of NREM stage 1 sleep, which has fairly low amplitude and a frequency of 8–12 Hz
type of brain wave characteristic of the end of stage 1 NREM sleep, which has a moderately low amplitude and a frequency of 4–7 Hz
second stage of sleep; the body goes into deep relaxation; characterized by the appearance of sleep spindles
rapid burst of high frequency brain waves during stage 2 sleep that may be important for learning and memory
very high amplitude pattern of brain activity associated with stage 2 sleep that may occur in response to environmental stimuli
third stage of sleep; deep sleep characterized by low frequency, high amplitude delta waves
type of brain wave characteristic during stage 3 NREM sleep, which has a high amplitude and low frequency of less than 3 Hz
people become aware that they are dreaming and can control the dream’s content
theory that dreams are the result of electrical impulses that pull random thoughts and imagery from our memories
one of a group of sleep disorders characterized by unwanted, disruptive motor activity and/or experiences during sleep
(also, somnambulism) sleep disorder in which the sleeper engages in relatively complex behaviors
sleep disorder in which the muscle paralysis associated with the REM sleep phase does not occur; sleepers have high levels of physical activity during REM sleep, especially during disturbing dreams
sleep disorder in which the sufferer has uncomfortable sensations in the legs when trying to fall asleep that are relieved by moving the legs
sleep disorder in which the sleeper experiences a sense of panic and may scream or attempt to escape from the immediate environment
sleep disorder defined by episodes during which breathing stops during sleep
sleep disorder in which the sufferer cannot resist falling to sleep at inopportune times
lack of muscle tone or muscle weakness, and in some cases complete paralysis of the voluntary muscles
changes in normal bodily functions that cause a drug user to experience withdrawal symptoms upon cessation of use
emotional, rather than a physical, need for a drug which may be used to relieve psychological distress
state of requiring increasing quantities of the drug to gain the desired effect
variety of negative symptoms experienced when drug use is discontinued
drug that tends to suppress central nervous system activity
drug that tends to increase overall levels of neural activity; includes caffeine, nicotine, amphetamines, and cocaine
one of a class of drugs that results in profound alterations in sensory and perceptual experiences, often with vivid hallucinations
type of amphetamine that can be made from pseudoephedrine, an over-the-counter drug; widely manufactured and abused
one of a category of drugs that has strong analgesic properties; opiates are produced from the resin of the opium poppy; includes heroin, morphine, methadone, and codeine
synthetic opioid that is less euphorigenic than heroin and similar drugs; used to manage withdrawal symptoms in opiate users
opiate with relatively low potency often prescribed for minor pain
one of a class of drugs that results in profound alterations in sensory and perceptual experiences, often with vivid hallucinations
state of extreme self-focus and attention in which minimal attention is given to external stimuli
clearing the mind in order to achieve a state of relaxed awareness and focus
