5.2 Environmental Risks
Learning Objectives
- Define teratogens and describe the factors that influence their effects
- List and describe the effects of several common teratogens
- Explain maternal and paternal factors that affect the developing fetus
- Explain the types of prenatal assessment
Teratology
Good prenatal care is essential for healthy development. The developing child is most at risk for severe problems during the first three months of development. Unfortunately, this is a time when many gestational parents are unaware that they are pregnant. Today, we know many of the factors that can jeopardize the health of the developing child. The study of factors that contribute to birth defects is called teratology. Teratogens are environmental factors that can contribute to birth defects, and include some parental diseases, pollutants, drugs and alcohol.
Factors influencing prenatal risks
There are several considerations in determining the kind and amount of damage that can result from exposure to a particular teratogen (Berger, 2005). These include:
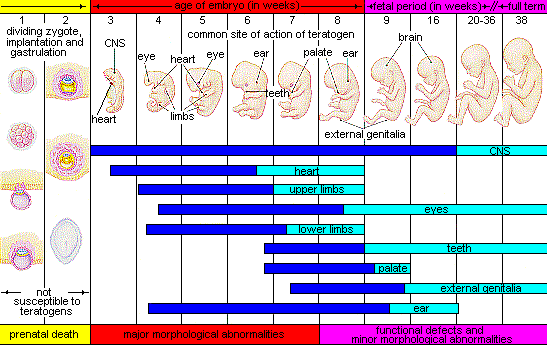
- The timing of the exposure. Structures in the body are vulnerable to the most severe damage when they are forming. If a substance is introduced during a particular structure’s critical period (time of development), the damage to that structure may be greater. For example, the ears and arms reach their critical periods at about 6 weeks after conception. If a gestational parent exposes the embryo to certain substances during this period, its ears and arms may be malformed.
- The amount of exposure. Some substances are not harmful unless the amounts reach a certain level. The critical level depends in part on the size and metabolism of the gestational parent.
- The number of teratogens. Fetuses exposed to multiple teratogens typically have more problems than those exposed to only one.
- Genetics. Genetic make-up also plays a role in the impact a particular teratogen has on a child. This is suggested by research showing that fraternal twins exposed to the same prenatal environment, do not always experience the same teratogenic effects. The genetic make-up of the gestational parent can also have an effect; some gestational parents may be more resistant to teratogenic effects than others.
- Being male or female. Males are more likely to experience damage due to teratogens than are females. It is believed that the Y chromosome, which contains fewer genes than the X, may make males more vulnerable.
Figure 5.8 illustrates the timing of teratogen exposure and the types of structural defects that can occur during the prenatal period.
Alcohol
One of the most common teratogens is alcohol, and because half of all pregnancies in the United States are unplanned, it is recommended that people of child-bearing age take great caution against drinking alcohol when not using birth control or when pregnant (CDC, 2005). Alcohol use during pregnancy is the leading preventable cause of intellectual disabilities in children in the United States (Maier & West, 2001). Alcohol consumption at any point during pregnancy, but particularly during the second month of prenatal development, may lead to neurocognitive and behavioral difficulties that can last a lifetime.
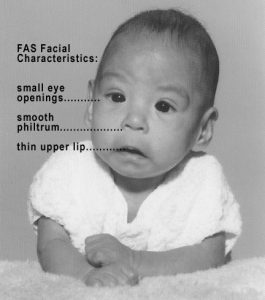
In extreme cases, alcohol consumption during pregnancy can lead to fetal death, but also can result in Fetal Alcohol Spectrum Disorders (FASD), which is an umbrella term for the range of effects that can occur due to alcohol consumption during pregnancy (March of Dimes, 2016a). The most severe form of FASD is Fetal Alcohol Syndrome (FAS). Children with FAS share certain physical features such as flattened noses, small eye holes, and small heads (see Figure 3.7). Cognitively, these children have poor judgment, poor impulse control, higher rates of ADHD, learning issues, and lower IQ scores. These developmental problems and delays persist into adulthood (Streissguth et al., 1996) and contribute to criminal behavior, psychiatric problems, and unemployment (CDC, 2016a). Based on animal studies, it has been hypothesized that a gestational parent’s alcohol consumption during pregnancy may predispose their child to like alcohol (Youngentob et al., 2007). Binge drinking, or 4 or more drinks in 2 to 3 hours, during pregnancy increases the chance of having a baby with FASD (March of Dimes, 2016a).
Watch It
Several medical experts debunk common myths about the safety of drinking alcohol during pregnancy.
You can view the transcript for “NOFAS Topics: Light Drinking” here (opens in new window).
Tobacco
Another widely used teratogen is tobacco; in fact, in 2016, more than 7% of pregnant women smoked in 2016 (Someji & Beltrán-Sánchez, 2019). According to Tong et al. (2013) in conjunction with the Centers for Disease Control and Prevention, data from 27 sites in 2010 representing 52% of live births, showed that among women with recent live births:
- About 23% reported smoking in the 3 months prior to pregnancy.
- Almost 11% reported smoking during pregnancy.
- More than half (54.3%) reported that they quit smoking by the last 3 months of pregnancy.
- Almost 16% reported smoking after delivery.
When comparing the ages of women who smoked:
- Women <20, 13.6% smoked during pregnancy
- Women 20–24 ,17.6% smoked during pregnancy
- Women 25–34 , 8.8% smoked during pregnancy
- Women ≥35, 5.7% smoked during pregnancy
The findings among racial and ethnic groups indicated that smoking during pregnancy was highest among American Indians/Alaska Natives (26.0%) and lowest among Asians/Pacific Islanders (2.1%).
When a pregnant person smokes, the fetus is exposed to dangerous chemicals including nicotine, carbon monoxide, and tar, which lessen the amount of oxygen available to the fetus. Oxygen is important for overall growth and development. Tobacco use during pregnancy has been associated with ectopic pregnancy (fertilized egg implants itself outside of the uterus), placenta previa (placenta lies low in the uterus and covers all or part of the cervix), placenta abruption (placenta separates prematurely from the uterine wall), preterm delivery, low birth weight, stillbirth, fetal growth restriction, sudden infant death syndrome (SIDS), birth defects, learning disabilities, and early puberty in girls (Center for Disease Control, 2015d).
When gestational parents are exposed to secondhand smoke during pregnancy, this also increases the risk of low-birth weight infants. In addition, exposure to thirdhand smoke, or toxins from tobacco smoke that linger on clothing, furniture, and in locations where smoking has occurred, can have a negative impact on infants’ lung development. Rehan et al. (2011) found that prenatal exposure to thirdhand smoke played a greater role in altered lung functioning than postnatal exposure.
Prescription/Over-the-counter Drugs
About 70% of pregnant people take at least one prescription drug (March of Dimes, 2016e). A person should not be taking any prescription medication during pregnancy unless it was prescribed by a health care provider who knows that person is pregnant. Some prescription drugs can cause birth defects, problems in overall health, and development of the fetus. Over-the-counter drugs are also a concern during the prenatal period because they may cause certain health problems. For example, the pain reliever ibuprofen can cause serious blood flow problems to the fetus during the last three months.
Illicit Drugs
Common illicit drugs include marijuana, cocaine, ecstasy and other club drugs, heroin, and prescription drugs that are abused. It is difficult to fully determine the effects of particular illicit drugs on a developing fetus because most gestational parents who take illicit drugs, frequently take more than one substance and have other unhealthy behaviors. These include smoking, drinking alcohol, not eating healthy meals, and being more likely to get a sexually transmitted disease.
However, several problems seem clear. The use of cocaine is connected with low birth weight, stillbirths, and spontaneous abortion (miscarriage). Heavy marijuana use is associated with problems in brain development (March of Dimes, 2016c). If a baby’s gestational parent used an addictive drug during pregnancy that baby can get addicted to the drug before birth and go through drug withdrawal after birth, also known as Neonatal abstinence syndrome (March of Dimes, 2015d). Other complications of illicit drug use include premature birth, smaller than normal head size, birth defects, heart defects, and infections. Additionally, babies born to gestational parents who use drugs may have problems later in life, including death from sudden infant death syndrome, slower than normal growth, and learning and behavior difficulties. Children of substance using parents are also considered at high risk for a range of biological, developmental, academic, and behavioral problems, including developing substance abuse problems of their own (Conners et al., 2003).
Link to Learning: Should People Who Consume Drugs During Pregnancy Be Arrested and Jailed?
People who take drugs or alcohol during pregnancy can cause serious lifelong harm to their children. Some people have advocated mandatory screenings for people who become pregnant and have a history of drug use, and if the people continue using, to arrest, prosecute, and incarcerate them (Figdor & Kaeser, 1998). This policy was tried in Charleston, South Carolina in 1989. The policy was called the Interagency Policy on Management of Substance Abuse During Pregnancy and had disastrous results.
The Interagency Policy applied to patients attending the obstetrics clinic at the Medical University of South Carolina, which primarily serves patients who are in poverty or on Medicaid. It did not apply to private obstetrical patients. The policy required patient education about the harmful effects of substance abuse during pregnancy. A statement also warned patients that protection of unborn and newborn children from the harms of illegal drug use could involve the Charleston police, the Solicitor of the Ninth Judicial Court, and the Protective Services Division of the Department of Social Services (DSS). (Jos et al., 1995, pp. 120–121).
Rather than helping newborns, this policy seemed to deter gestational parents from seeking prenatal care and to deter them from seeking other social services. And because this policy was applied solely to low-income people, it also resulted in lawsuits. The program was canceled after 5 years, during which time 42 gestational parents were arrested. A federal agency later determined that the program involved human experimentation without the approval and oversight of an institutional review board (IRB).
In July 2014, Tennessee enacted a law that allows people who illegally use a narcotic drug while pregnant to be prosecuted for assault if her infant is harmed or addicted to the drug (National Public Radio, 2015). According to the National Public Radio report, a baby is born dependent on a drug every 30 minutes in Tennessee, which is a rate three times higher than the national average. However, since the law took effect the number of babies born having drug withdrawal symptoms has not diminished. Critics contend that the criminal justice system should not be involved in what is considered a healthcare problem. What do you think? Do you consider the issue of gestational parents using illicit drugs more of a legal or a medical concern?
Pollutants
There are more than 83,000 chemicals used in the United States with little information on their effects on unborn children (March of Dimes, 2016b).
- Lead poisoning. An environmental pollutant of significant concern is lead, which has been linked to fertility problems, high blood pressure, low birth weight, prematurity, miscarriage, and delayed neurological development. Grossman and Slutsky (2017) found that babies born in Flint Michigan, an area identified with high lead levels in the drinking water, were premature, weighed less than average, and gained less weight than normal.
- Pesticides. Chemicals in certain pesticides are also potentially damaging and may lead to miscarriage, low birth weight, premature birth, birth defects, and learning problems, (March of Dimes, 2014).
- Bisphenol A. Prenatal exposure to bisphenol A (BPA), a chemical commonly used in plastics and food and beverage containers, may disrupt the action of certain genes contributing to particular birth defects (March of Dimes, 2016b).
- Radiation. If a gestational parent is exposed to radiation, it can get into the bloodstream and pass through the umbilical cord to the fetus. Radiation can also build up in body areas close to the uterus, such as the bladder. Exposure to radiation can cause result in miscarriage, affect brain development, slow the baby’s growth, or cause birth defects or cancer.
- Mercury. Mecury, a heavy metal, can cause brain damage and affect the baby’s hearing and vision. This is why people are cautioned about the amount and type of fish they consume during pregnancy.

Toxoplasmosis
The tiny parasite, toxoplasma gondii, causes an infection called toxoplasmosis. According to the March of Dimes (2012d), toxoplasma gondii infects more than 60 million people in the United States. A healthy immune system can keep the parasite at bay resulting in no symptoms, so most people do not know they are infected. As a routine prenatal screening frequently does not test for the presence of this parasite, pregnant people may want to talk to their health-care provider about being tested. Toxoplasmosis can cause premature birth, stillbirth, and can result in birth defects to the eyes and brain. While most babies born with this infection show no symptoms, ten percent may experience eye infections, enlarged liver and spleen, jaundice, and pneumonia. To avoid being infected, gestational parents should avoid eating undercooked or raw meat and unwashed fruits and vegetables, touching cooking utensils that touched raw meat or unwashed fruits and vegetables, and touching cat feces, soil, or sand. If people think they may have been infected during pregnancy, they should have their newborn tested.
Sexually transmitted diseases
Gonorrhea, syphilis, and chlamydia are sexually transmitted infections that can be passed to the fetus by an infected gestational parent. Gestational parents should be tested as early as possible to minimize the risk of spreading these infections to their unborn children. Additionally, the earlier the treatment begins, the better the health outcomes for parent and baby (CDC, 2016d). Sexually transmitted diseases (STDs) can cause an ectopic pregnancy, miscarriage, premature rupture of the amniotic sac, premature birth, still births. and birth defects (March of Dimes, 2013). Although some STDs can cross the placenta and infect the developing fetus, most babies become infected with STDS while passing through the birth canal during delivery.
Human Immunodeficiency Virus (HIV)
One of the most potentially devastating teratogens is HIV. One of the main ways children under age 13 become infected with HIV is via mother-to-child transmission of the virus prenatally, during labor, or by breastfeeding (CDC, 2016c). There are measures that can be taken to lower the chance the child will contract the disease. HIV positive gestational parents who take antiviral medications during their pregnancy greatly reduce the chance of passing the virus to the fetus. The risk of transmission is less than 2%; in contrast, if the gestational parent does not take antiretroviral drugs, the risk is elevated to 25% (CDC, 2016b). However, the long-term risks of prenatal exposure to the medication are not known. It is recommended that people with HIV deliver the child by c-section, and that after birth they avoid breast feeding.
German measles (or rubella)
Rubella, also called German measles, is an infection that causes mild flu-like symptoms and a rash on the skin. Rubella in the gestational parent has been associated with a number of birth defects. If the gestational parent contracts the disease during the first three months of pregnancy, damage can occur in the eyes, ears, heart or brain of the unborn child. if the pregnant person has German measles before the 11th week of prenatal development, deafness is almost certain and brain damage can also result. People in the United States are much less likely to be afflicted with rubella, because most receive childhood vaccinations which protect them from the disease.
Maternal Factors
Gestational parent over 35
Most people over 35 who become pregnant are in good health and have healthy pregnancies. However, according to the March of Dimes (2016d), people over age 35 have an increased risk of:
- Fertility problems
- High blood pressure
- Diabetes
- Miscarriages
- Placenta Previa
- Cesarean section
- Premature birth
- Stillbirth
- A baby with a genetic disorder or other birth defects
Because a gestational parent is born with all their eggs, environmental teratogens can affect the quality of the eggs as they get older. Also, their reproductive system ages which can adversely affect the pregnancy. Some people over 35 choose special prenatal screening tests, such as a maternal blood screening, to determine if there are any health risks for the baby.

Although there are medical concerns associated with having a child later in life, there are also many positive consequences to being a more mature parent. Older parents are more confident, less stressed, and typically married, which can provide family stability. Their children perform better on math and reading tests, and they are less prone to injuries or emotional troubles (Albert, 2013). People who choose to wait are often well educated and lead healthy lives. According to Gregory (2007), older women are more stable, demonstrate a stronger family focus, possess greater self-confidence, and have more money. Having a child later in one’s career equals overall higher wages. In fact, for every year a gestational parent delays becoming a parent, they make 9% more in lifetime earnings. Lastly, gestational parents who delay having children actually live longer. Sun et al. (2015) found that women who had their last child after the age of 33 doubled their chances of living to age 95 or older than women who had their last child before their 30th birthday. A gestational parent’s natural ability to have a child at a later age indicates that their reproductive system is aging slowly, and consequently so is the rest of their body.
Teenage pregnancy
A teenage gestational parent is at a greater risk for complications during pregnancy, including anemia and high blood pressure. These risks are even greater for those under age 15. Infants born to teenage gestational parents have a higher risk of being born prematurely and having low birthweight or other serious health problems. Premature and low birthweight babies may have organs that are not fully developed which can result in breathing problems, bleeding in the brain, vision loss, and serious intestinal problems. Very low birthweight babies (less than 3 1/3 pounds) are more than 100 times as likely to die, and moderately low birthweight babies (between 3 1/3 and 5 ½ pounds) are more than 5 times as likely to die in their first year, than normal weight babies (March of Dimes, 2012c). Again, the risk is highest for babies of gestational parents under age 15. A primary reason for these health issues is that teenagers are the least likely of all age groups to get early and regular prenatal care. Additionally, they may engage in risky behaviors during pregnancy, including eating unhealthy food, smoking, drinking alcohol, and taking drugs. Additional concerns for teenagers are repeat births. About 25% of teen gestational parents under age 18 have a second baby within 2 years after the first baby’s birth.
Gestational diabetes
Seven percent of pregnant people develop gestational diabetes (March of Dimes, 2015b). Diabetes is a condition where the body has too much glucose in the bloodstream. Most pregnant people have their glucose level tested at 24 to 28 weeks of pregnancy. Gestational diabetes usually goes away after the gestational parent gives birth, but it might indicate a risk for developing diabetes later in life. If untreated, gestational diabetes can cause premature birth, stillbirth, infant breathing problems at birth, jaundice, or low blood sugar. Babies born to mothers with gestational diabetes can also be considerably heavier (more than 9 pounds) making the labor and birth process more difficult. For expectant mothers, untreated gestational diabetes can cause preeclampsia (high blood pressure and signs that the liver and kidneys may not be working properly) discussed later in the chapter. Risk factors for gestational diabetes include age (being over age 25), being overweight or gaining too much weight during pregnancy, a family history of diabetes, having had gestational diabetes with a prior pregnancy, and race and ethnicity (mothers who are African-American, Native American, Hispanic, Asian, or Pacific Islander have a higher risk). Eating healthy food and maintaining a healthy weight during pregnancy can reduce the chance of gestational diabetes. People who already have diabetes and become pregnant need to attend all their prenatal care visits, and follow the same advice as those for people with gestational diabetes as the risk of preeclampsia, premature birth, birth defects, and stillbirth are the same.
High blood pressure (Hypertension)
Hypertension is a condition in which the pressure against the wall of the arteries becomes too high. There are two types of high blood pressure during pregnancy, gestational and chronic. Gestational hypertension only occurs during pregnancy and goes away after birth. Chronic high blood pressure refers to people who already had hypertension before the pregnancy or to those who developed it during pregnancy and it continued after birth. According to the March of Dimes (2015c) about 8 in every 100 pregnant people have high blood pressure. High blood pressure during pregnancy can cause premature birth and low birth weight (under five and a half pounds), placental abruption, and mothers can develop preeclampsia.
Rh disease
Rh is a protein found in the blood. Most people are Rh positive, meaning they have this protein. Some people are Rh negative, meaning this protein is absent. Gestational parents who are Rh negative are at risk of having a baby with a form of anemia called Rh disease (March of Dimes, 2009). A father who is Rh-positive and gestational parent who is Rh-negative can conceive a baby who is Rh-positive. Some of the fetus’s blood cells may get into the gestational parent’s bloodstream and their immune system is unable to recognize the Rh factor. The immune system starts to produce antibodies to fight off what it thinks is a foreign invader. Once the pregnant person’s body produces immunity, the antibodies can cross the placenta and start to destroy the red blood cells of the developing fetus. As this process takes time, often the first Rh positive baby is not harmed, but because the pregnant person’s body continues to produce antibodies to the Rh factor across their lifetime, subsequent pregnancies can pose greater risk for an Rh positive baby. In newborns, Rh disease can lead to jaundice, anemia, heart failure, brain damage and death.
Weight gain during pregnancy
According to March of Dimes (2016f) during pregnancy most people need only an additional 300 calories per day to aid in the growth of the fetus. Gaining too little or too much weight during pregnancy can be harmful. People who gain too little may have a baby who is low-birth weight, while those who gain too much are likely to have a premature or large baby. There is also a greater risk for the gestational parent developing preeclampsia and diabetes, which can cause further problems during the pregnancy. Table 5.1 shows the healthy weight gain during pregnancy. Putting on the weight slowly is best. Gestational parents who are concerned about their weight gain should talk to their health care provider.
Table 5.1 Weight gain during pregnancy
| If you were a healthy weight before pregnancy | If you were underweight before pregnancy | If you were overweight before pregnancy | If you were obese before pregnancy |
| • gain 25-35lbs • 1-4½lbs in the first trimester and 1lb per week in the second and third trimesters |
• gain 28-40lbs • 1-4½lbs in the first trimester and a little more than 1lb per week thereafter |
• gain 12-25 lbs • 1-4½lbs in the first trimester and a little more than ½lb per week in the second and third trimesters |
• 11-20lbs • 1-4½lbs in the first trimester and less than ½lb per week in the second and third trimesters |
| Gestational parents of multiples need to gain more in each category |
Stress
It is common to feel stressed during pregnancy, but high levels of stress can cause complications including having a premature or low-birthweight baby. Babies born early or too small are at an increased risk for health problems. Stress-related hormones may cause these complications by affecting a gestational parent’s immune systems resulting in an infection and premature birth. Additionally, some people deal with stress by smoking, drinking alcohol, or taking drugs, which can lead to problems in the pregnancy. High levels of stress in pregnancy have also been correlated with problems in the baby’s brain development and immune system functioning, as well as childhood problems such as trouble paying attention and anxiety (March of Dimes, 2012b).
Depression
Depression is a significant medical condition in which feelings of sadness, worthlessness, guilt, and fatigue interfere with one’s daily functioning. Depression can occur before, during, or after pregnancy, and 1 in 7 pregnant people are treated for depression sometime between the year before pregnancy and the year after pregnancy (March of Dimes, 2015a). People who have experienced depression previously are more likely to have depression while pregnant. Consequences of depression include the baby being born prematurely, having a low birthweight, being more irritable, less active, less attentive, and having fewer facial expressions. About 13% of pregnant people take an antidepressant during pregnancy. It is important that pregnant people taking antidepressants discuss the medication with a health care provider as some medications can cause harm to the developing organism. In fact, birth defects are about 2 to 3 times more likely in people who are prescribed certain Selective Serotonin Reuptake Inhibitors (SSRIs) for their depression.
Link to Learning: Reducing the Risk
Did you know that gestational parents can improve outcomes for themselves and their babies through a balanced diet and adequate exercise? Click through this interactive to learn more about the importance of the gestational parent’s health.

Paternal impact
The age of fathers at the time of conception is also an important factor in health risks for children. According to Nippoldt (2015) offspring of men over 40 face an increased risk of miscarriage, autism, birth defects, achondroplasia (bone growth disorder) and schizophrenia. These increased health risks are thought to be due to chromosomal aberrations and mutations that accumulate during the maturation of sperm cells in older men (Bray et al., 2006). However, like older women, the overall risks are small.
In addition, men are more likely than women to work in occupations where hazardous chemicals, many of which have teratogenic effects or may cause genetic mutations, are used (Cordier, 2008). These may include petrochemicals, lead, and pesticides that can cause abnormal sperm and lead to miscarriages or diseases. Men are also more likely to be a source of secondhand smoke for their developing offspring. As noted earlier, smoking by either the mother or around the gestational parent can impede prenatal development.
Try It
References (Click to expand)
Albert, E. (2013). Many more women delay childbirth into 40s due to career constraints. Milwaukee Journal Sentinel. Retrieved from http://www.jsonline.com/news/health/many-more-women-delay-childbirth-into-40s-due-to-career-constraints-b9971144z1-220272671.html
Bray, I., Gunnell, D., & Smith, G. D. (2006). Advanced paternal age: How old is too old? Journal of Epidemiology & Community Health, 60(10), 851-853. Doi: 10.1136/jech.2005.045179
Centers for Disease Control and Prevention. (2005). Surgeon’s general’s advisory on alcohol use during pregnancy. Retrieved from https://www.cdc.gov/ncbddd/fasd/documents/surgeongenbookmark.pdf
Centers for Disease Control and Prevention. (2016a). Fetal alcohol spectrum disorders. Retrieved from http://www.cdc.gov/ncbddd/fasd
Centers for Disease Control and Prevention. (2016b). HIV/AIDS prevention. Retrieved from http://www.cdc.gov/hiv/basics/prevention.html
Centers for Disease Control and Prevention. (2016c). HIV transmission. Retrieved from http://www.cdc.gov/hiv/basics/transmission.html
Centers for Disease Control and Prevention. (2016d). STDs during pregnancy. Retrieved from http://www.cdc.gov/std/pregnancy/stdfact-pregnancy.htm
Centers for Disease Control and Prevention. (2015d). Smoking, pregnancy, and babies. Retrieved from http://www.cdc.gov/tobacco/campaign/tips/diseases/pregnancy.html
Conners, N.A., Bradley, R.H., Whiteside-Mansell, L., Liu, J.Y., Roberts, T.J., Burgdorf, K., & Herrell, J.M. (2003). Children of mothers with serious substance abuse problems: An accumulation of risks. The American Journal of Drug and Alcohol Abuse, 29 (4), 743–758.
Cordier, S. (2008). Evidence for a role of paternal exposure in developmental toxicity. Basic and Clinical Pharmacology and Toxicology, 102, 176-181.
Figdor, E., & Kaeser, L. (1998). Concerns mount over punitive approaches to substance abuse among pregnant women. The Guttmacher report on public policy, 1(5), 3–5.
Gregory, E. (2007). Ready: Why women are embracing the new later motherhood. Philadelphia, PA: Basic Books.
Grossman, D., & Slutsky, D. (2017). The effect of an increase in lead in the water system on fertility and birth outcomes: The case of Flint, Michigan. Economics Faculty Working Papers Series. Retrieved from http://www2.ku.edu/~kuwpaper/2017Papers/201703.pdf
Jos, P. H., Marshall, M. F., & Perlmutter, M. (1995). The Charleston policy on cocaine use during pregnancy: A cautionary tale. The Journal of Law, Medicine, and Ethics, 23(2), 120-128.
Maier, S.E., & West, J.R. (2001). Drinking patterns and alcohol-related birth defects. Alcohol Research & Health, 25(3), 168-174.
March of Dimes. (2009). Rh disease. Retrieved from http://www.marchofdimes.org/complications/rh-disease.aspx
March of Dimes. (2012a). Rubella and your baby. Retrieved from http://www.marchofdimes.org/baby/rubella-and-your-baby.aspx 68
March of Dimes. (2012b). Stress and pregnancy. Retrieved from http://www.marchofdimes.org/pregnancy/stress-and-pregnancy.aspx
March of Dimes. (2012c). Teenage pregnancy. Retrieved from http://www.marchofdimes.org/materials/teenage-pregnancy.pdf
March of Dimes. (2012d). Toxoplasmosis. Retrieved from http://www.marchofdimes.org/complications/toxoplasmosis.aspx
March of Dimes. (2013). Sexually transmitted diseases. Retrieved http://www.marchofdimes.org/complications/sexually-transmitted-diseases.aspx
March of Dimes. (2014). Pesticides and pregnancy. Retrieved from http://www.marchofdimes.org/pregnancy/pesticides-and-pregnancy.aspx
March of Dimes. (2015a). Depression during pregnancy. Retrieved from http://www.marchofdimes.org/complications/depression-during-pregnancy.aspx
March of Dimes. (2015b). Gestational diabetes. Retrieved from http://www.marchofdimes.org/complications/gestational-diabetes.aspx
March of Dimes. (2015c). High blood pressure during pregnancy. Retrieved from http://www.marchofdimes.org/complications/high-blood-pressure-during-pregnancy.aspx
March of Dimes. (2015d). Neonatal abstinence syndrome. Retrieved from http://www.marchofdimes.org/complications/neonatal-abstinence-syndrome-(nas).aspx
March of Dimes. (2016a). Fetal alcohol spectrum disorders. Retrieved from http://www.marchofdimes.org/complications/fetal-alcohol-spectrum-disorders.aspx
March of Dimes. (2016b). Identifying the causes of birth defects. Retrieved from http://www.marchofdimes.org/research/identifying-the-causes-of-birth-defects.aspx
March of Dimes. (2016c). Marijuana and pregnancy. Retrieved from http://www.marchofdimes.org/pregnancy/marijuana.aspx
March of Dimes. (2016d). Pregnancy after age 35. Retrieved from http://www.marchofdimes.org/pregnancy-after-age-35.aspx
March of Dimes. (2016e). Prescription medicine during pregnancy. Retrieved from http://www.marchofdimes.org/pregnancy/prescription-medicine-during-pregnancy.aspx
March of Dimes. (2016f). Weight gain during pregnancy. Retrieved from http://www.marchofdimes.org/pregnancy/weight-gain-during-pregnancy.aspx
National Public Radio. (Producer). (2015, November 18). In Tennessee, giving birth to a drug-dependent baby can be a crime [Audio podcast]. Retrieved from http://www.npr.org/templates/transcript.php?storyld=455924258
Nippoldt, T.B. (2015). How does paternal age affect a baby’s health? Mayo Clinic. Retrieved from http://www.mayoclinic.org/healthy-lifestyle/getting-pregnant/expert-answers/paternal-age/faq– 20057873
Rehan, V. K., Sakurai, J. S., & Torday, J. S. (2011). Thirdhand smoke: A new dimension to the effects of cigarette smoke in the developing lung. American Journal of Physiology: Lung Cellular and Molecular Physiology, 301(1), L1-8.
Someji, S., & Beltrán-Sánchez, H. (2019). Association of maternal cigarette smoking and smoking cessation with preterm birth. JAMA Network Open, 2(4), e192514. doi:10.1001/jamanetworkopen.2019.2514
Streissguth, A.P., Barr, H.M., Kogan, J. & Bookstein, F. L. (1996). Understanding the occurrence of secondary disabilities in clients with Fetal Alcohol Syndrome (FAS) and Fetal Alcohol Effects (FAE). Final Report to the Centers for Disease Control and Prevention (CDC), August. Seattle: University of Washington, Fetal Alcohol & Drug Unit, Tech. Rep. No. 96-06.
Sun, F., Sebastiani, P., Schupf, N., Bae, H., Andersen, S. L., McIntosh, A., Abel, H., Elo, I., & Perls, T. (2015). Extended maternal age at birth of last child and women’s longevity in the Long Life Family Study. Menopause: The Journal of the North American Menopause Society, 22(1), 26-31.
Tong, V. T., Dietz, P.M., Morrow, B., D’Angelo, D.V., Farr, S.L., Rockhill, K.M., & England, L.J. (2013). Trends in smoking before, during, and after pregnancy — Pregnancy Risk Assessment Monitoring System, United States, 40 Sites, 2000–2010. Surveillance Summaries, 62(SS06), 1-19. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/ss6206a1.htm
Youngentob, S. L., Molina, J. C., Spear, N. E., & Youngentob, L. M. (2007). The effect of gestational ethanol exposure on voluntary ethanol intake in early postnatal and adult rats. Behavioral Neuroscience, 121(6), 1306-1315. doi.org/10.1037/0735-7044.121.6.1306
Licenses & Attributions (Click to expand)
CC Licensed Content
- “Beginnings: Conception and Prenatal Development” by Human Development Teaching & Learning Group is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License
- “Lifespan Development: A Psychological Perspective, Second Edition” by Martha Lally and Suzanne Valentine-French is licensed under a CC-BY-NC-SA-3.0
- “Environmental Risks during Prenatal Development” by Julie Lazzara for Lumen Learning is licensed under a CC BY: Attribution
Media Attributions
- criticalperiods © Laura Overstreet is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Photo_of_baby_with_FAS © Teresa Kellerman is licensed under a CC BY-SA (Attribution ShareAlike) license
- catbox © Tom Thai is licensed under a CC BY (Attribution) license
- camylla-battani-son4VHt4Ld0-unsplash © Camylla Battani is licensed under a CC0 (Creative Commons Zero) license
- Hazardous-pesticide © Unknown is licensed under a Public Domain license
All Rights Reserved Content
- NOFAS Topics: Light Drinking. Provided by: AlcoholFreePregnancy. Located at: https://www.youtube.com/watch?time_continue=231&v=pvFqjU43Odo. License: Other. License Terms: Standard YouTube License
